Types of TAPVR
Total anomalous pulmonary venous return is classified into different types. This is based on how and where the pulmonary veins drain to the heart:
Supracardiac Total Anomalous Pulmonary Venous Return
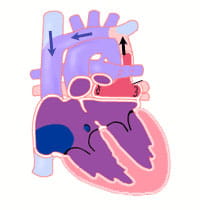
The pulmonary veins drain to the right atrium by the superior vena cava. In this type of TAPVR, the pulmonary veins come together behind the heart and then drain upwards to an abnormal “vertical vein.” This vertical vein joins the innominate vein which connects to the right superior vena cava and drains to the right atrium.
Cardiac Total Anomalous Pulmonary Venous Return
The pulmonary veins come together behind the heart. They then drain to the right atrium through the coronary sinus. The coronary sinus is the vein that normally returns blood from the heart muscle itself back to the right atrium after its oxygen has been used. The coronary sinus drains directly into the right atrium.
Infracardiac Total Anomalous Pulmonary Venous Return
The pulmonary veins drain to the right atrium by the hepatic (liver) veins and inferior vena cava. In this type, the pulmonary veins join together behind the heart. They then drain downwards, connecting to the liver's portal vein system. They drain through the vascular bed of the liver and enter the right atrium from the hepatic veins.
All types of total anomalous pulmonary venous return must have an atrial septal defect (ASD). An ASD is a hole in the wall between the right and left upper chambers of the heart. This hole will allow some of the oxygenated blood that has entered the right atrium from the pulmonary vein to go across to the left atrium and out to the body.
Associated Problems
Because of the abnormal pulmonary vein connection red (oxygenated) blood returning from the lungs mixes with the blue (lower oxygenated) blood returning from the body.
The left side of the heart (left atrium and left ventricle) is filled only by mixed blood. Because this blood is a mixture of red and blue (oxygenated and deoxygenated) blood, the overall oxygen content is decreased in the blood leaving the heart and going to the body. This is why patients with TAPVR have low oxygen saturations.
If the atrial septal defect (ASD) is small or limits blood flow from the right atrium to the left atrium, then the volume of blood filling the left atrium and left ventricle may be lessened. This can lead to low blood supply to the body and shock.
In some cases of TAPVR, the route of blood from the pulmonary veins back to the heart may have areas of narrowing or obstruction. This obstruction may stop a normal amount of blood return from the pulmonary veins. It may increase the pressure in the veins. Blockage in the pulmonary veins leads to congestion in the lungs (pulmonary edema, or excessive fluid) and pulmonary hypertension (high pressure in the lung vessels).
Patients with obstructed TAPVR are critically ill with severe cyanosis and often have very unstable blood pressure. Surgery may be needed right away for these patients.
Obstructed pulmonary veins commonly occur in the infracardiac type of TAPVR. It can occur with the other anatomic types as well.
Signs and Symptoms
Patients with obstructed total anomalous pulmonary venous return (TAPVR) are ill soon after birth. These children are severely cyanotic (blue coloring to skin, lips and nails). They also have respiratory problems, rapid breathing, grunting and retractions of the rib cage muscles.
If obstruction to pulmonary venous return is not present, children with TAPVR may not have many symptoms. There may be some fast breathing or trouble breathing. There is often cyanosis. It may be mild and hard to see.
Some children with this more common type of TAPVR are diagnosed when a doctor hears a heart murmur during a physical examination. These children may not be diagnosed for several weeks to months.
Diagnosis
The diagnosis of total anomalous pulmonary venous return may be suspected when a doctor hears a typical heart murmur. They may see evidence of overload on the right side of the heart.
Oxygen saturations may be low in children without pulmonary venous obstruction. An electrocardiogram (ECG) may be helpful to show if there are problems with enlargement of the heart.
A chest X-ray will show enlargement of the right side of the heart. In newborns with TAPVR and obstructed pulmonary venous return, chest X-ray may show signs of pulmonary edema (fluid in the lungs).
The diagnosis of TAPVR is made by echocardiogram (echo). This study will show the abnormal connection of the pulmonary veins.
Echocardiography (echo) will also show if the right atrium and right ventricle are larger than normal. It can show the size of and flow across the atrial septal defect (ASD).
Sometimes cardiac catheterization is needed to make a diagnosis of TAPVR.
Cardiac catheterization will define the abnormal connection of all pulmonary veins. This is helpful finding unusual patterns of mixed TAPVR.
Cardiac catheterization can also accurately determine whether pulmonary veins are obstructed. It can see if the atrial septal defect is “restrictive” (too small). If the ASD is restrictive, a balloon dilation procedure can be done to enlarge the defect.
Treatment
Total anomalous pulmonary venous return is a defect that needs surgery to fix. The timing of the surgical repair varies depending on the type of TAPVR present. The condition of the child is considered as well
Surgery is done right away for newborns with obstructed TAPVR. Some of these children will need extracorporeal life support (ECMO) prior to surgery because of their blood flow instability.
Children with TAPVR without obstruction have surgery days to weeks after the diagnosis is made.
Rarely, TAPVR is complicated by a restrictive atrial septal defect. This means the hole in the atrial septum is not big enough to let enough blood through to the left side. In these children, a balloon dilation procedure may be done at cardiac catheterization. This will improve the child's condition before surgery.
The surgical repair connects all of the veins to the back of the left atrium. This leads to a normal connection of pulmonary veins to left atrium. All other routes for pulmonary venous drainage are tied off.
Finally, the atrial septal defect (ASD) is also closed.
Outcomes and Long-Term Outlook
The outcome of surgical repair for total anomalous pulmonary venous return is excellent. The surgical mortality is less than 5% when repair is performed electively. This is in healthy children without obstructed pulmonary veins.
The surgical mortality (death rate) is higher when surgery is done on an emergency basis on critically ill newborns with obstructed pulmonary venous. Critically ill newborns who do survive the surgery may need a long period of post-operative intensive care. They often are on a ventilator (breathing machine) as their lungs recover.
The long-term outcome after surgical repair of TAPV is also excellent. Because the surgical repair results in a normal circulation, these children are expected to grow and develop normally.
Rare complications of TAPVR can occur late after surgery. Regular follow up by a qualified cardiologist is needed to detect these problems early if they occur.
Rarely, obstruction to one or more pulmonary veins can develop. This can occur at the site of surgical repair, or due to abnormalities of the pulmonary veins themselves. Such pulmonary vein obstruction can lead to a shortness of breath or wheezing. The diagnosis can be somewhat hard to make. It may need cardiac catheterization to diagnose.
Abnormal cardiac rhythm is another late complication of TAPVR. It is also rare. Because of the extensive atrial surgery involved in the repair, some patients can have abnormal electrical impulses in the atrium.
When these impulses occur in single beats, they are typically benign. They do not need any treatment. On rare occasion, patients can have either continuous episodes of rapid heartbeat, or slow heart rates. Either sustained fast heart rates or slow heart rates may need treatment. The results of treatment (either medical or with a pacemaker) are excellent.
TAPVR Management in Adults and Adolescents
Patients who have surgery to repair total anomalous pulmonary venous return early in their lives often do well. Most do not need expert follow-up care as adults.
Learn more about the Adolescent and Adult Congenital Heart Disease Program.