Evidence-Based Decision Making
Evidence-Based Decision Making
Cincinnati Children’s believes in and practices evidence-based decision making (EBDM) as a way to achieve the best, safest care for children. Patients, purchasers, regulators and others expect practice to be based on sound judgment and best evidence; however, the proportion of clinical practice that has a basis in published scientific research is lower than one would expect. And the time it takes to translate new research findings into clinical practice can take years.
With this in mind, Cincinnati Children’s designed a division within the James M. Anderson Center for Health Systems Excellence to promote, support and spread EBDM to the point of care. The value of EBDM was recognized when the Board of Trustees incorporated evidence initiatives into the medical center’s strategic plan, making it our mission to be the leader in evidenced-based care locally, regionally and around the world.
How We Define Evidence-Based Decision Making
All these components are included in evidence-based decision making (EBDM) and shared decision making (SDM).
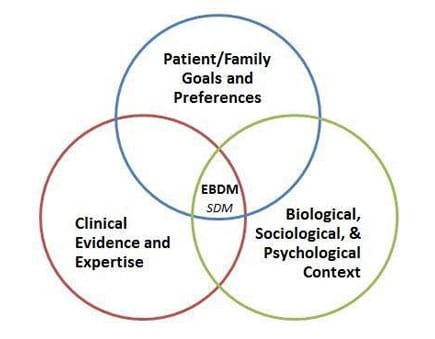
Clinical evidence and expertise together shape the options that are clinically reasonable.
- Clinical evidence is the use of studies that help define best practices in a clinical setting. Clinical expertise is the use of clinical skills with experience in practice that informs daily decisions.
Patient / family goals and preferences shape the options that hold value for the patient / family.
- Each patient and family is unique. Eliciting patient / family goals and preferences informs clinicians about what is most important to families.
The biological, sociological and psychological contexts shape the options that are most relevant for the individual patient and family.
- Insight into these contexts can help clinicians tailor care to match the situation of each patient and family.
Shared decision making is a process that involves clinicians communicating information about treatment options, and patients and parents communicating the personal value they place on the trade-offs involved so that agreement on the best strategy for the patient can be reached.
Evidence-based decision making is a process in which care decisions are optimized by bringing all of these perspectives together.
How We Promote Evidence
Our evidence group has focused on several key processes and resources to support EBDM throughout the medical center:
Rapid Evidence Adoption to Improve Child Health (REACH)
Horizon scanning, evidence synthesis (e.g., rapid evidence reviews), embedding evidence and measuring and spreading evidence adoption are used to close the gap between evidence generation or publication and use of the evidence in decision making at the point of care.
Shared Decision Making (SDM)
Evidence-based tools are used to facilitate clinicians' communication about treatment options and patients / parents' communication about the personal value they place on the trade-offs involved. The goal is to reach agreement on the best strategy for a patient when there are two or more medically reasonable options differing in ways that are important to families.
Evidence Evaluation Tools & Resources (LEGEND)
We collaborated with groups from nursing (patient services), allied health (occupational therapy / physical therapy), hospital medicine and our medical research library to develop the LEGEND (Let Evidence Guide Every New Decision) system, standardizing EBDM education and evidence evaluation for the institution. This system includes tools and resources for proceeding through the evidence evaluation process, including critically appraising individual studies, grading the body of evidence and judging the strength of recommendation statements.
Evidence-Based Care Recommendations
- Best evidence statements: We use best evidence statements to improve recommendation development and streamlined evidence reviews to improve revision processes.
- Evidence-based care guidelines: We develop and disseminate high-quality processes and products, primarily evidence-based guidelines.



