Standardized Pediatric Intensive Care Unit (PICU) Mortality
Why we measure:
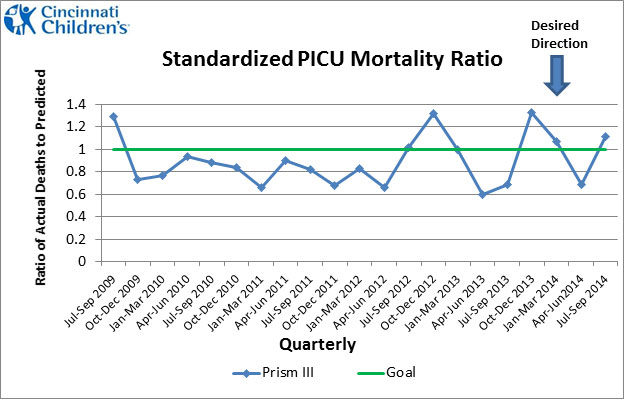
- This measure uses an established method to calculate predicted mortality. Predicted mortality is a way to measure how likely a child is to die based upon how sick he or she is. A number less than 1.0 indicates that mortality for a given time period is LESS than would have been predicted. A number greater than 1.0 indicates that mortality for a given time period is GREATER than would have been predicted. The blue line shows our current performance.
- Although Standardized PICU Mortality looks specifically at the outcomes of patients cared for in one specific unit (PICU), the measure assesses the service delivery system as a whole and hospital quality beyond just the PICU. Key healthcare activities including initial evaluation, timely and accurate communication of important information from provider to provider, and ongoing assessment and treatment planning, all contribute to performance on this measure.
Click here to view a larger version of the chart in PDF format.
How we measure:
- Standardized PICU Mortality Ratio is measured as the ratio of actual deaths over predicted deaths for PICU patients. The number of predicted deaths is calculated during the first 12 hours of a PICU stay using the Pediatric Risk of Mortality (Prism III) score. This score takes into account how sick a child is using 17 physiologic variables such as vital signs and results of certain laboratory tests.
- Monitoring and improvement on this measure began in April 2003. In July 2013, Cincinnati Children’s transitioned from Prism II to the newest version of the algorithm, Prism III. Prism III contains several updates including enhanced age adjustment and additional risk factors that combined produce a more accurate model for mortality risk.
- An archived chart compares performance using the Prism II and the Prism III algorithms. The more sophisticated algorithms and risk adjustment of Prism III provide a clearer picture of performance and mortality risk. Moving forward, Prism III will be used to monitor performance and inform ongoing improvement efforts.
What we are doing to improve:
- We continually monitor this measure and use it as a signal for when more detailed analysis and additional follow-up may be warranted.
- We contribute data to Virtual PICU Systems, LLC (“VPS”). VPS participating hospitals commit to the collection of high quality data elements that are used to understand, evaluate and improve care and outcomes for critically ill children. Through this participation we have access to standardized data sharing for improved patient care, research and benchmarking among pediatric ICUs.
- No one intervention is the primary driver of performance. PICU standardized mortality results and sustained performance are attributed to a combination of safety improvement interventions. This includes an intense focus on the reliable implementation of care bundles to prevent infections for patients with central venous catheters, patients who are on ventilators and patients who undergo surgical procedures. We also attribute our focus on reducing serious safety events, early recognition and mitigation of patient deterioration, safe hand-offs, and multidisciplinary and PICU physician-led rounds, as part of the combination of efforts to continually improve and keep patients safe.
View the Operational Definition: Standardized PICU Mortality



