Tiny Particles, Big Medicine: New Proton Therapy Center Will Transform Cancer Care, Trigger a Wave of Discovery
Research By: John Perentesis, MD
Post Date: June 29, 2019 | Publish Date: Fall 2016

“The capabilities of this facility will bring together collaborators from a wide realm of expertise—including investigators from outside Cincinnati Children’s—whose work will take proton therapy to a new level.”
—John Perentesis, MD
In a world where advances in medical technology tend to be measured in microns and nanograms, the idea of cancer research leaping forward through the installation of equipment weighing more than 280 tons seems almost absurd.
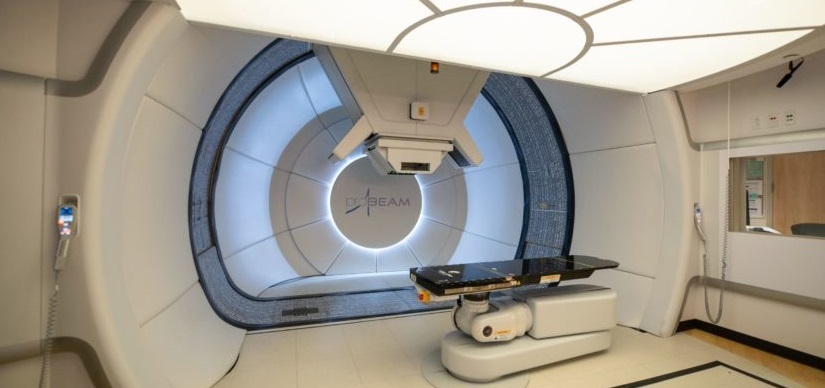
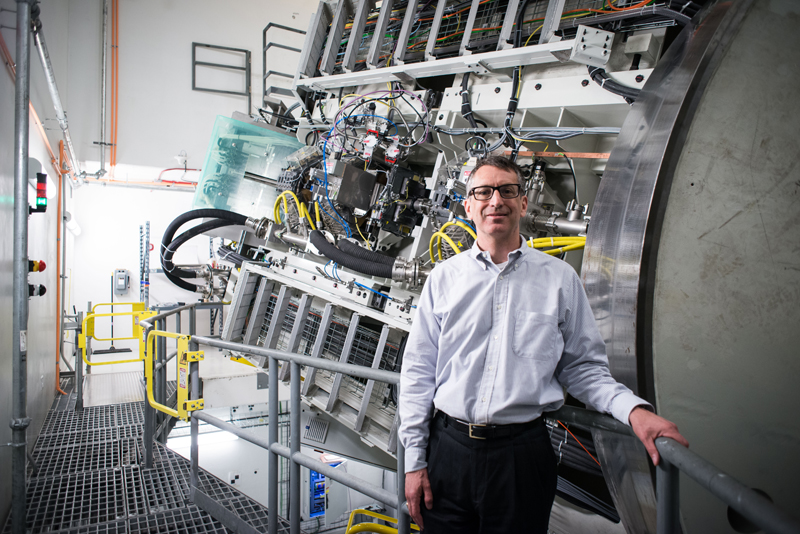
Yet that’s how much just one of the precision guiding gantries at Cincinnati Children’s new Proton Therapy Center weighs. And once the facility reaches full-service capacity this fall, it will have three of these behemoths – including the world’s only proton treatment gantry dedicated exclusively to research and development.
This is big medicine intended to make a big difference.
The Proton Therapy Center’s grand opening later this month caps off more than a decade of planning, an investment approaching $120 million, and a three-year construction project that involved 31,000 yards of concrete and more than 155 miles of wiring. The first patients will begin receiving treatments in September, soon to be followed by a swarm of research initiatives.
“This center will become a national anchor for particle-based cancer research,” says John Perentesis, MD, Co-Executive Director, Cancer and Blood Diseases Institute. “The capabilities of this facility will bring together collaborators from a wide realm of expertise – including investigators from outside Cincinnati Children’s – whose work will take proton therapy to a new level.”

TRANSFORMING RADIATION THERAPY
Across the U.S., about one-quarter of all children diagnosed with cancer receive radiotherapy as part of their care. These treatments have contributed to rapid improvements in cure rates. However, the price of progress has included children surviving brain tumors, but growing up with cognitive impairment; or beating Hodgkin lymphoma only to face heart disease caused by stray radiation.
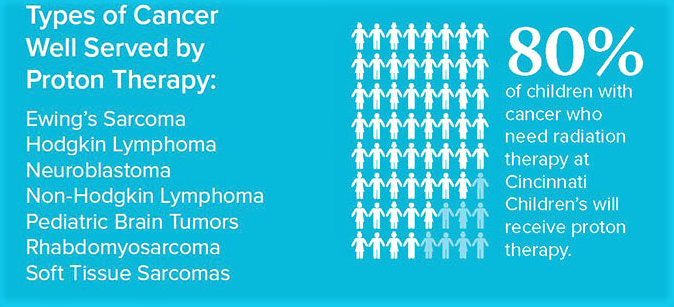
Proton therapy is applicable for more than 80 percent of children in need of radiation therapy as part of their treatment regimen. For many cancer survivors, the result will be growing up with far fewer risks of long-term consequences.
“Even with all the work that goes into making conventional radiotherapy as safe as possible, we know that as much as one-third of the radiation dose a patient receives can wind up deposited away from the targeted tumor,” Perentesis says. “Unfortunately for some children, this can lead to some immediate side effects and secondary cancers and other side effects developing as much as 25 to 30 years after treatment. We expect proton therapy to dramatically reduce these risks.”
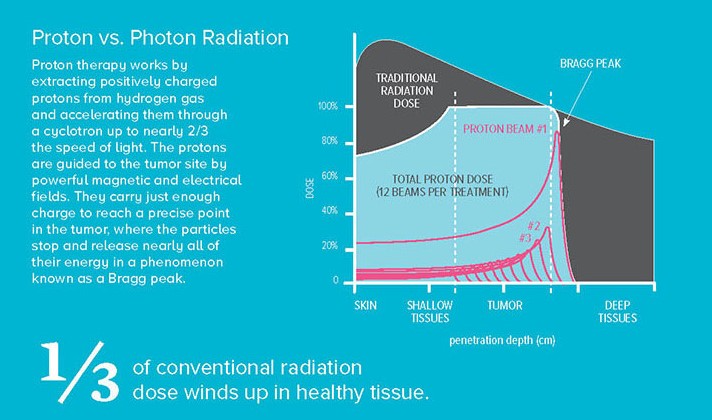
Proton therapy reduces risk by sending particles into the body at relatively low levels of radiation, which then stop within the targeted tissue to release nearly all their energy in a spike of output known as a Bragg peak. The photon energy from conventional X-ray beams passes all the way through tissue, killing the targeted cancer cells but also damaging healthy tissue on the way in and out. View an animation of how Proton Therapy works for cancer treatment.
FINE TUNING AN EMERGING TOOL
Proton therapy already represents a significant step forward. However, much more research is needed to refine the technology. “There is still so much we do not yet understand about the biological effects of proton therapy,” Perentesis says.
Susanne Wells, PhD, directs the Epithelial Carcinogenesis and Stem Cell Program at Cincinnati Children’s. She is part of a growing team of experts from Cincinnati Children’s and the University of Cincinnati (UC) who are launching proton-related research projects.
“We want to be as sophisticated as possible in making use of the tremendous resources that we have,” Wells says. “We are employing genomics, metabolomics and other large-scale approaches to get down to the details of proton radiation biology. All of these aspects have been vastly understudied in comparison to conventional photon radiation.”
AN AMBITIOUS AGENDA
Research planned for the Proton Therapy Center will follow several tracks, including:
Basic biological research: How exactly do protons kill cancer cells? Scientists have long studied how ionizing radiation from photons disrupts DNA and causes cell death. But few have yet taken deep dives into the genetic and molecular pathways that protons can affect.
The scientific literature already reports, for example, that RNA responses differ when a cell is radiated with photons, protons or carbon ions. This has potential far-reaching implications for determining the most effective doses for specific types of cancer occurring in specific types of tissue.
One of several projects seeking to shed light along these lines will involve isolating cancer stem cells from the rest of a tumor, then testing that population’s reaction to proton vs. photon radiation.
Applied research and development: Currently, proton devices magnetically bend proton streams into pencil-like beams that can paint a tumor, layer by layer, with tiny bursts of radiation. The cell-killing damage can be confined to less than a millimeter of tissue.
Yet as impressive as that may be, even more precision is desired. When patients receive as many as 40 treatment sessions across several weeks, a variety of critical events can occur. Children grow. People lose or gain weight. The tumor itself can shift – and hopefully – shrink as treatment progresses, being replaced by healthy tissues.
The research gantry at Cincinnati Children’s will serve as a real-world test platform for evaluating imaging methods, computer targeting technologies, patient positioning techniques, and more. The goal: improve treatment plans created and updated at specific points in time into an even more flexible approach that keeps constant precise track of the size and location of a tumor.
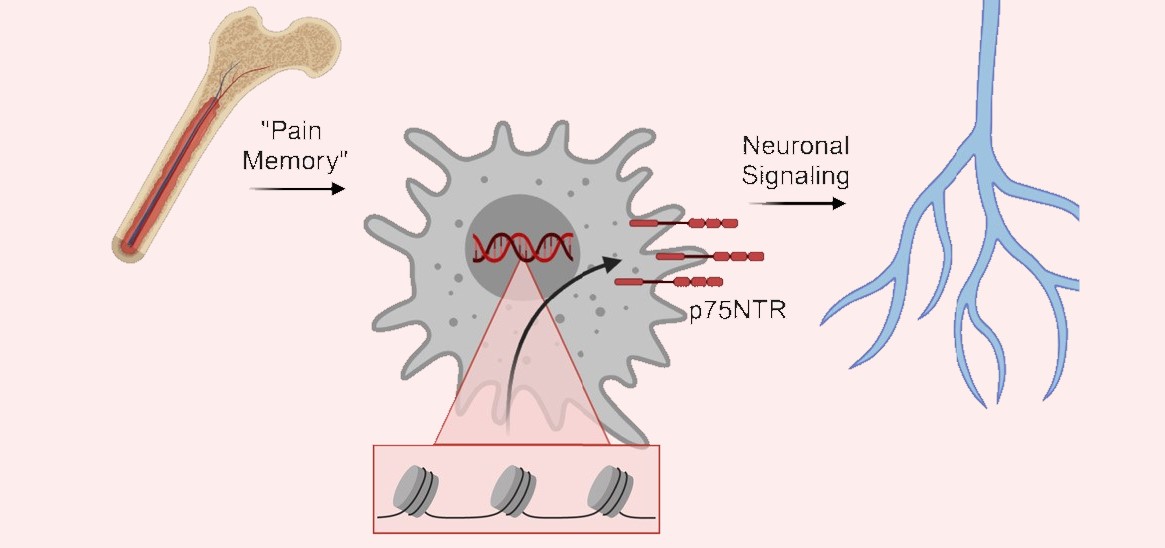
Translational research: A major goal for proton research here is to develop and refine radio-sensitizing treatments that can augment proton therapy. These are drugs that can be given in conjunction with radiation treatments that increase the likelihood of cell death when hit by radiation. A number of such agents already exist, but their effects can vary with the types of cancer and radiation source, and few of these properties have been documented for children.
How proton therapy can work best in conjunction with evolving chemotherapy regimens and emerging immune therapy approaches remains to be explored. Engineering experts at UC are especially interested in exploring nanoparticles that could make it easier to target cancer cells or fortify healthy tissues near a tumor site.
NEXT STEPS
Proton research will be conducted in cooperation with various departments at UC, the University of Cincinnati Physicians, the University of Cincinnati Medical Center, and Varian, the equipment manufacturer. Some collaborations also involve research centers in Germany and Israel, and more multi-institutional partnerships are likely.
Initial funding comes from the institutions involved, with the goal of seeking larger grants from the National Cancer Institute, the National Science Foundation, and other sources as pilot projects demonstrate progress.
“Ultimately, the clinical goal is to figure out which people will be most responsive to proton therapy,” Wells says. “What tumors, which individuals will benefit the most?”
—By Tim Bonfield
(This article originally appeared in the Fall 2016 issue of Research Horizons)
Research By