Developing a Clinical-Grade Vector
Our core laboratories make it possible
Few pediatric hospitals are able to handle every stage of producing the gene therapy for a Phase I/II clinical trial such as the sickle cell study. Cincinnati Children’s exceptional core laboratories support every stage of cell-based therapy, from developing the vector through its use in patients and follow up testing to evaluate effectiveness.
 Johannes van der Loo, PhD |
Choosing the Vector
The treatment that will be used in the sickle cell clinical trial began many years ago with the choice of the vector, which serves as the transport medium to deliver the treatment to the cells. Years of research have taught that viruses make good vectors.
Lentivirus was chosen as the vector for this trial because it can handle the large size of the hemoglobin gene being transferred and allows permanent integration of the gene into the target cells. Our scientists modified the virus to remove all potentially harmful genes and any genes that would result in a virus infection.
“The only gene the vector will transfer to the patient’s cells is the gene we have engineered to be part of the trial,” says Han van der Loo, PhD. Van der Loo directs the Vector Production Facility at Cincinnati Children’s. He and his team have spent two years perfecting the manufacturing process of vector for the sickle cell trial.
 |
“Our challenge was to figure out how to best capture, purify and concentrate the virus, and make enough to serve the clinical trial,” says van der Loo.
Once van der Loo and his team were satisfied that the vector process was working as it should, a clinical batch of vector was prepared and samples were sent to outside facilities to be tested for potency, purity and safety. Testing is extensive, and everything hinges on the results.
“FDA approval is based on the lab’s ability to produce this safely and effectively,” van der Loo says. “We have to provide the material at the proper purity and strength for the doctors to do their investigation which is key to the trial.”
When the Trial Begins
Once the trial starts, another of Cincinnati Children’s core laboratories, the Cell Manipulation Laboratory (CML), takes over. Carolyn Lutzko, PhD, and Diana Nordling co-direct the CML.
 Carolyn Lutzko, PhD |
Nordling will oversee what happens in the clinical laboratory from the time the patient’s bone marrow — roughly a quart of it — is removed until the vector is
added and the marrow is re-injected into the patient.
“Our job is to make the procedure as safe as possible,” says Lutzko, who came to Cincinnati Children’s two years ago to work on this project. “We have to move everything into an environment and a method that can be used in humans.” She and her development team have performed dozens of trial runs to make sure the processing method goes smoothly.
It works like this: the patient’s bone marrow will be brought to the clinical lab within 20 to 30 minutes after it is removed. For the next 48 hours, a team working around the clock in a highly controlled environment will isolate the blood stem cells and will twice add the vector that holds the healthy genes produced by van der Loo’s group.
Is It Working?
 Diana Nordling |
Nordling’s role is also to ensure FDA requirements for gene therapy are met, which includes extensive testing throughout the procedure to determine if things are working as they should. “We collect the cells and do a lot of testing to make sure the product is safe and it’s what we expect,” she says.
What they expect is that the healthy blood cells with the modified gene will enter the patient’s stem cells and start taking over.
“During the processing we will be looking to see, are the cells alive, are there enough, is the product still free of contamination?” says Nordling.
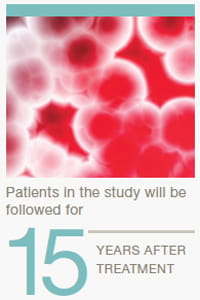
It could be weeks or months before doctors see evidence of the therapy’s effectiveness. Patient samples will continue to be analyzed at regularly scheduled visits to determine if the fetal hemoglobin is present, and in what quantity. Patients who participate in the study will be followed for 15 years after treatment.
The hope is that those 15 years will be without an incident of sickle cell disease.



