Learning Networks (Carole Lannon, MD, MPH, Faculty Lead)
Learning Networks are multisite collaborations that engage patients, families, clinicians and researchers to improve care and outcomes for children. The five networks supported by Cincinnati Children's Hospital Medical Center connect 412 clinical teams from 271 pediatric and maternity hospitals, including 43 states and three countries. Additional networks are in the design or early implementation phase. These Learning Networks provide collaborative laboratories that have identified effective clinical bundles, developed and tested shared decision-making tools, assessed dissemination and implementation strategies, used comparative effectiveness design to understand effective therapies, analyzed social network and used factorial design to identify dose-response of effective therapies. The five networks have over 60 publications to date. Specific research efforts and results include:
- The Children’s Hospitals’ Solutions for Patient Safety (SPS) Network has found that when hospitals reliably implement recommended care bundle elements, there are significant reductions in hospital acquired conditions (HACs). Therefore, evidence-based best practices have now identified and created for six pediatric HACs as well as Readmissions. The SPS Network is working with hospitals to spread and implement these bundles in care delivery in order to accelerate the pace of harm reduction.
The SPS Network highlights the SPS SSI Prevention Bundle in a recent Pediatrics publication titled, “Surgical Site Infection Reduction by the Solutions for Patient Safety Hospital Engagement Network.” The publication shows how adoption of a SSI prevention bundle, with concomitant reliability measurement, reduced the SPS Network’s SSI rate, and how linking reliability measurement to standardization at an institutional level may lead to safer care (Schaffzin, et al., Pediatrics, 2015 136(5):e1353-60).
The SPS Network receives funding in part from the Cardinal Health Foundation and Children’s Hospital Association.
- The Ohio Perinatal Quality Collaborative’s (OPQC) Neonatal Abstinence Syndrome (NAS) Project focuses on reducing preterm births and improving perinatal and preterm newborn outcomes in Ohio. Specifically, this quality improvement collaborative across 54 NICUs in Ohio has applied a factorial design approach in the project’s second phase to further reduce the length of stay for babies with Neonatal Abstinence Syndrome (NAS). The “factorial design of non-pharmacologic interventions for opioid addicted infants” is work produced from the NAS Project.
- The ImproveCareNow (ICN) learning health system is currently engaged in over 15 studies on such research questions as:
- Impact of patient-reported outcomes on treatment management
- Healthcare disparities in pediatric Crohn's disease
- Pediatric uveitis in the IBD population
- Anti-TNF monotherapy and other therapies
Perhaps most significantly, ICN awarded its largest clinical research award ever in April 2015, and kicked off the study in 2016: a $7.9 million Patient Centered Outcomes Research Institute (PCORI) grant for a five-year pragmatic clinical trial to compare Anti-TNF Monotherapy versus Combination Therapy with Low Dose Methotrexate in Pediatric Crohn’s Disease. The study is known as COMBINE (Clinical Outcomes of Methotrexate Binary treatment with INfliximab or adalimumab in practicE).
- During this past year, the National Pediatric Quality Improvement Collaborative (NPC-QIC) has realized several important accomplishments:
- Cumulative interstage mortality has decreased from 9.5% to 5.1%, a relative reduction of 46%.
- The percentage of infants experiencing growth failure has decreased from 18.6% to13.1%, a relative reduction of 28%.
- Significant reduction in infants readmittance to the hospital for serious medical problems across the collaborative.
The hard work of the now 60 centers has resulted in a wealth of knowledge about the best way to care for these complex infants, and to achieve better outcomes. To summarize the outcomes, we created an infographic documenting the collaborative’s success updated and published quarterly on our website; and to synthesize the identified best practices, we have created an Interstage Change Package document, available to assist teams in improving their care and outcomes.
- With support from a Center for Education and Research in Therapeutics (CERTs) mini-grant from AHRQ, and in collaboration with the Cincinnati Children's Center for Adherence & Self Management, the care centers of the Pediatric Rheumatology Care and Outcomes Improvement Network (PR-COIN) developed and tested a patient self-management support toolkit and training program. PR-COIN plans to develop a self-management handbook for JIA, as well as a pediatric self-management change package and self-management video.
The Anderson Center Learning Networks Core has external collaborations with the American Board of Pediatrics, the Autism Treatment Network, the national Children’s Hospital Association, the Ohio Children’s Hospital Association, the Ohio Hospital Association, the Ohio Department of Health, and the Ohio Department of Medicaid.
Within Cincinnati Children's, network partnerships connect the Anderson Center Learning Networks Core with the Divisions of Developmental and Behavioral Pediatrics; Endocrinology; Gastroenterology, Hepatology and Nutrition; General and Community Pediatrics; Nephrology and Hypertension; Pulmonary Medicine; Rheumatology; and the Cancer and Blood Diseases Institute; the Heart Institute; and the Perinatal Institute.
Funding for the networks comes from the Agency for Healthcare Research and Quality, the Centers for Education and Research on Therapeutics, the Centers for Disease Control and Prevention (CDC), the Children’s Heart Association of Cincinnati, Ohio Department of Health, Ohio Department of Medicaid, PICORI and fees from participating institutions. The Learning Networks Core project received a FY16 Cincinnati Children's Academic and Research Committee award to further develop the infrastructure to support existing and emergent networks.
Health Services Research (Peter Margolis, MD, PhD, Faculty Lead)
Faculty in the James M. Anderson Center for Health Systems Excellence do research across a broad range of health services research topics, but the emphasis tilts towards interventions–the design, implementation and testing of complex interventions to improve health and care delivery. Our focus is on developing a community of well-trained health services researchers who work together with patients and clinicians to answer their most important questions, embedding research into care delivery and creating efficient health services research infrastructure. Over the past year, research revenue has continued to grow, with a diversity of funding sources including federal, foundation and state support. Research includes large scale studies including the Ohio Perinatal Quality Collaborative (funded by Ohio Medicaid); Solutions for Patient Safety (CMS); developing a national research infrastructure through the Patient Centered Outcomes Research Institute (PCORI) Patient Powered Research Networks (ImproveCareNow and PR-COIN/PARTNERS); and a PCORI Clinical Data Research Network (PEDSnet). These networks are resulting in multiple studies focused on improvement science and the creation of important data sharing capability across multiple institutions. There are also numerous health services research projects taking place at Cincinnati Children's focused on a diverse range of topics and engaging investigators from more than 15 divisions. Topics include hospital and ambulatory safety, formal studies of dissemination and implementation approaches, technology enabled tools to promote patient engagement, methods to support N of 1 studies, data visualization and situational awareness. Robust faculty development support continues with over 15 faculty participating, and quality scholars from a diverse range of divisions. New areas of emphasis are the use of formal design methods to support the development of learning health systems.Safety Research (Kathleen Walsh, MD, Research Lead; Stephen Muething, MD, Operational Lead)
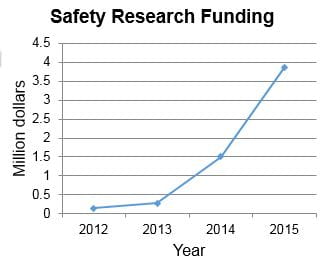
Research on patient and staff safety has had tremendous growth over the past four years, fueled by successful cross-divisional and interdisciplinary collaborations. Safety research proposal have been funded to investigators in nephrology, neonatology, hospital medicine, patient services, biomedical informatics, and the James M. Anderson Center for Health Systems Excellence. Investigators obtained funding from a variety of federal sources including the National Library of Medicine, the Eunice Kennedy Shriver National Institute of Child Health Development, and the Agency for Healthcare Research and Quality.
Several projects have focused on patient and family engagement in patient safety. Patrick Brady, MD, MSc, Division of Hospital Medicine, was awarded a K08 award entitled “Family Clinician Partnerships to Improve Child Safety in the Hospital”. In a collaboration between the James M. Anderson Center for Health Systems Excellence, the Center for Adherence Center and Self-Management, CBDI, and Research in Patient Services, Drs. Kathleen Walsh, Ahna Pai, Nancy Daraiseh, and John Perentesis were awarded an R01 to use home visits to study factors associated with medication errors and adherence in children with cancer. In a collaboration with hematology, Drs. Lori Crosby in the Center for Adherence Center and Self-Management, and Kathleen Walsh are developing and testing interventions to support hydroxyurea use at home, supported by a Place Outcomes Award.
Finally, in a collaboration between quality improvement, topic experts, and health services research, Drs. Stuart Goldstein, Steve Muething, and Kathleen Walsh received and R18 from AHRQ to study the spread of NINJA to eight other hospitals nationally. “While there was more up-front work to think through how to use our different backgrounds in basic science research, quality improvement, and health services research together, this project which is will to advance nephrology and patient safety would not have been possible without such collaboration.” The safety research program is an excellent example of success that comes through multidisciplinary collaboration.



