Automated System Predicts Children at High Risk for Acute Kidney Injury
Published May 2022 | Kidney International Reports
Research led by Stuart Goldstein, MD, and colleagues integrates the Renal Angina Index (RAI) developed at Cincinnati Children’s with an automated clinical decision support program to improve its ease of use at the bedside.
A three-year prospective trial called TAKING FOCUS 2 (TF2) is testing the program. First-year TF2 data demonstrated improved prediction of severe acute kidney injury (AKI) when the urinary biomarker neutrophil gelatinase-associated lipocalin (NGAL) is evaluated in critically ill patients with an RAI ≥8.
TF2 integrates the RAI into the Epic™ electronic medical record. Epic™ automatically calculates the RAI at the first 12 hours of admission to the pediatric intensive care unit (PICU). If the RAI ≥8, a clinician simply releases a reflex order for an NGAL test. Clinicians use the results to guide treatment, which can include fluid management and renal replacement therapy initiation.
Goldstein hopes that the TF2 study leads to the universal availability of an automated RAI tool that clinicians everywhere can use.
AKI occurs in about 25% of critically ill children admitted to the PICU. Severe AKI occurs in 11% of PICU cases and is independently associated with morbidity and 28-day mortality. The RAI-NGAL clinical decision support system lets clinicians quickly guide therapy for patients likely to develop severe AKI and avoid unnecessary interventions for patients not likely to develop AKI.
The system “provides real-time data that helps intensivists and nephrologists support patients with severe AKI in a standardized way earlier than they did before,” Goldstein says.
TAKING FOCUS 2 AKI
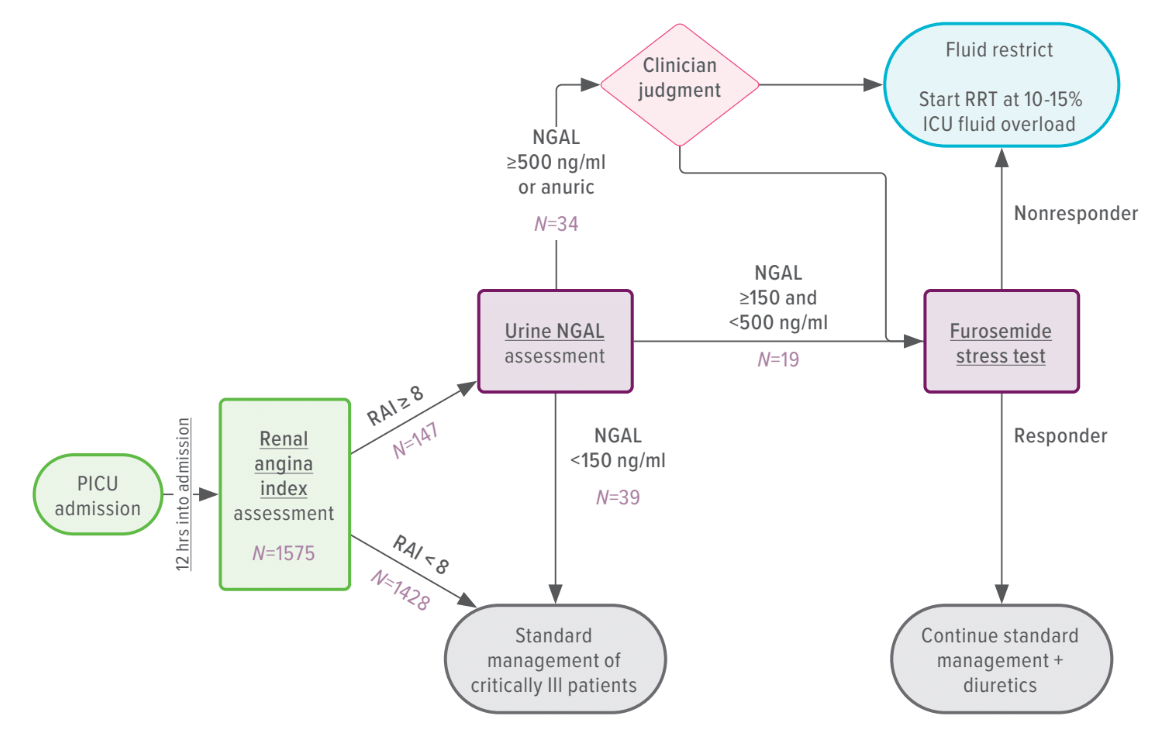
The TAKING FOCUS 2 AKI clinical decision support flow algorithm can predict whether a child will develop severe AKI within three days of admission to the pediatric intensive care unit and can guide physicians in applying treatment. The clinical support algorithm suggests patients at low risk, RAI− and RAI+/NGAL−, receive standard management per PICU. Patients at high risk, RAI+/NGAL+, with NGAL 150−500 ng/ml, can have further risk stratification with a furosemide stress test (FST), unless contraindicated, whereas those with >500 ng/ml can either have an FST or initiate renal replacement therapy (RRT) if there is an emergent indication or if it is deemed better/urgent by the primary team. FST responders have a lower risk of requiring RRT, so management with diuretic and fluid restriction is suggested, although FST nonresponders are likely to fail diuretic management and an initiation of RRT is suggested if FO >10% to 15% cannot be prevented by fluid restriction alone.