For children with a kidney transplant, heart disease is the biggest threat to their long-term health1-3. There are many reasons, including their underlying kidney disease, being on dialysis, and the medications they must take to prevent their body from rejecting their new kidney. Cincinnati Children’s has led the way in identifying many heart disease risk factors for children who have had a kidney transplant, and we systematically track and treat these risk factors in our patients.
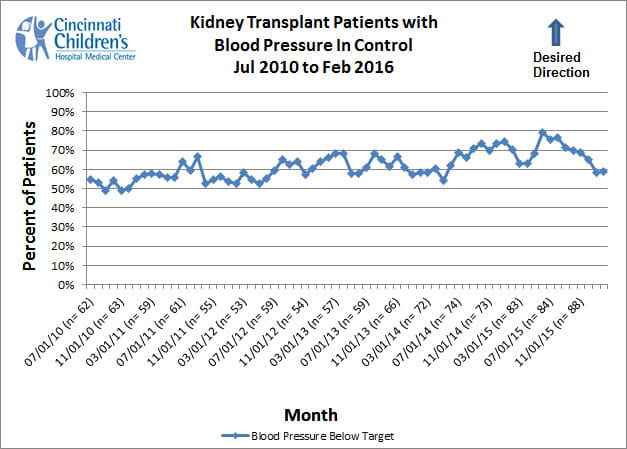
Blood Pressure Control
High blood pressure (also called hypertension) is perhaps the most important risk factor for heart disease in kidney transplant patients. Up to 80 percent of children with a kidney transplant have a diagnosis of hypertension4. Even though there are many effective therapies to treat hypertension, many children with a kidney transplant have poorly controlled blood pressure5, 6. The blood pressure control measure shows the proportion of patients under our care whose blood pressure is adequately treated according to national guidelines.
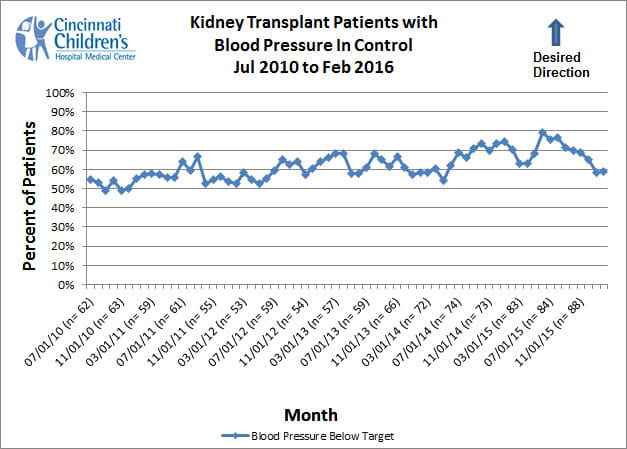
How We Measure
We include all patients who have been seen in our clinic within the last six months and whose kidney transplant was at least three months before calculating each data point. A patient’s blood pressure is considered to be adequately controlled if it is below 120 / 80 and below the 90th percentile for age, gender, and height for patients under 18 years old, or if it is below 130 / 80 for patients 18 years of age or older7, 8.
Continuous Improvement
It is very important to measure blood pressure correctly or the results might be inaccurate. Based on an extensive review of available research, we have developed a Best Evidence Statement (BESt) for the proper Blood Pressure Measurement in Children. We have worked to implement this procedure and are happy to report that nearly 100 percent of kidney transplant patients have their blood pressure measured appropriately at each clinic visit.
- By maintaining optimal blood pressure, a kidney transplant will last longer, the heart will be healthier and the patient will feel better. At Cincinnati Children’s, our approach to improving blood pressure control includes several essential components including accurate measurement, planned medical care, state-of-the-art therapy (including medication management, self-management, diet and lifestyle interventions, and collaboration with the Adherence Center), and assessment of effects of high blood pressure on the heart and kidney, including echocardiography and measurement of renal function.
- We use the latest technology to closely monitor blood pressure and ensure that it remains within optimal ranges. In addition to thoroughly measuring blood pressure in clinic, we also ask patients to monitor blood pressure at home. This gives us additional information that can be used to develop a treatment plan tailored to each patient.
- Before every clinic visit, we review patients’ most recent blood pressure readings and other heart disease risk factors so we are ready with a personalized plan even before patients arrive for their visit.
- In addition to drug therapy, our treatment approach consists of diet and lifestyle counseling and follow-up with a registered dietitian.
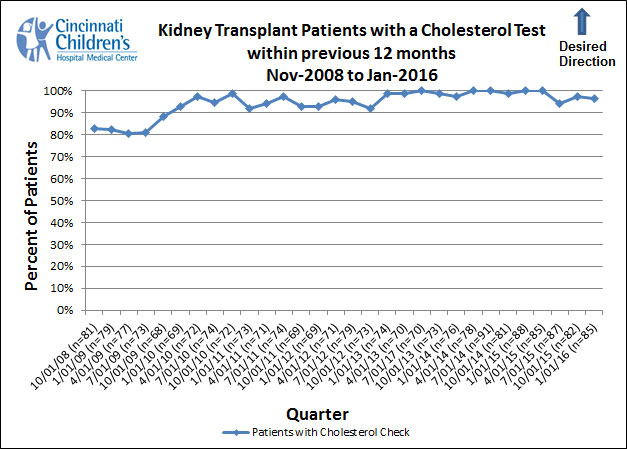
Cholesterol Monitoring and Control
High cholesterol is another important heart disease risk factor for children with a kidney transplant. Up to 80 percent of children will have or develop high cholesterol following kidney transplantation4 that may add to the risk of heart disease in the future.
The cholesterol monitoring within the previous 12 months measure illustrates the proportion of patients in our entire population who have had their cholesterol checked within the previous year.
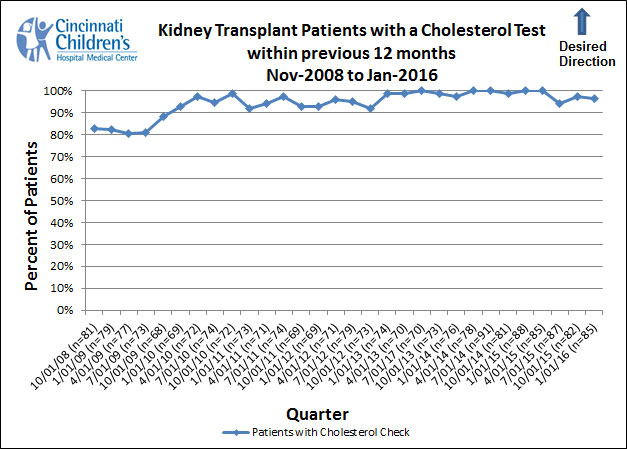
How We Measure
We include all patients who have been seen in our clinic within the previous 12 months and who had their transplant more than seven months earlier.
Continuous Improvement
- At Cincinnati Children’s, we measure cholesterol at least once a year in all our patients and more often for patients with the highest risk for high cholesterol. Through the use of automated reporting systems, we can identify the patients who are most at risk, and monitor their cholesterol accordingly.
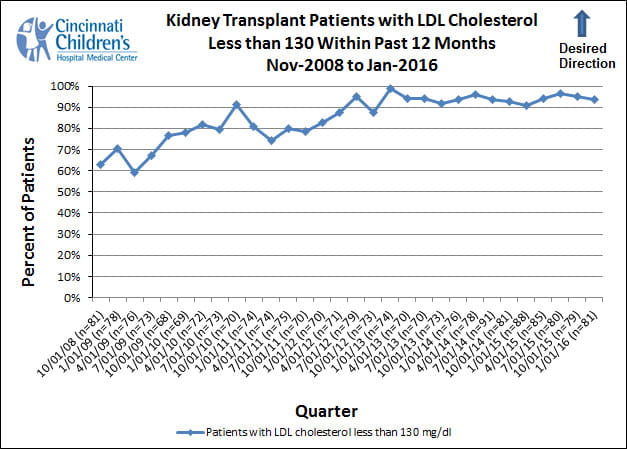
The low density lipoprotein (LDL) cholesterol control measure illustrates the proportion of patients in our population who had LDL documented as controlled within the prior 12 months, according to national recommendations8, 9.
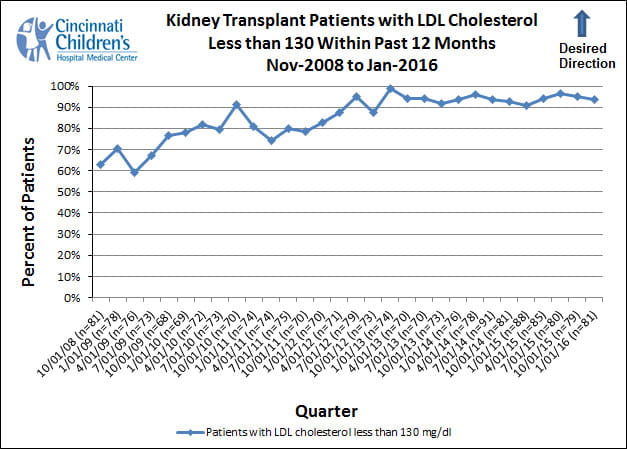
How We Measure
We include all patients who have been seen in our clinic within the previous 12 months and who had their transplant more than seven months earlier. The measure reports the proportion of all patients who had controlled LDL at their most recent check within the last 12 months. The national recommended guideline is that LDL be below 130 mg / dl8, 9.
- Our approach to treating high cholesterol includes a team of providers consisting of transplant pharmacologists, nurses, registered dietitians, and the patient’s physician. When treating high cholesterol, we use a variety of interventions including assessment of whether medications that cause high cholesterol can be stopped, counseling and regular follow-up with a registered dietitian about maintaining a heart-healthy diet and lifestyle, and consideration of medications that have been proven effective in lowering cholesterol.
- All of the treatment options mentioned above are considered during our pre-visit planning meetings with the treatment team. Each member of the team is trained in motivational interviewing and self-management techniques to support patients in making lifestyle changes that will lead to better health.