Liver Transplantation – Quality Measures
Accurately measuring and critically reviewing outcomes data are the first steps in continuous quality improvement. Our liver transplant team is committed to not only reviewing, but sharing our outcomes with patients, families and the transplant community. We believe this philosophy helps create an open, collaborative environment in which sharing of knowledge and best practices will improve the care for all children undergoing liver transplantation.
U.S. News & World Report consistently ranks the Division of Gastroenterology at Cincinnati Children’s among the nation’s top programs in its annual guide of “Best Children’s Hospitals.”
Integral to the gastroenterology program is the Liver Transplant Program. To achieve the best outcomes, we have assembled dedicated teams that track a variety of measures, each aimed at improving care before and after liver transplantation. Measures we currently report include:
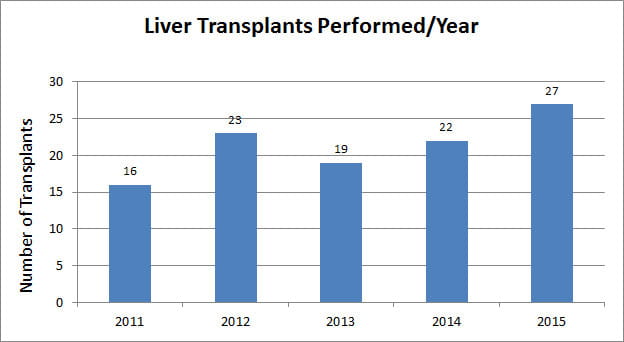
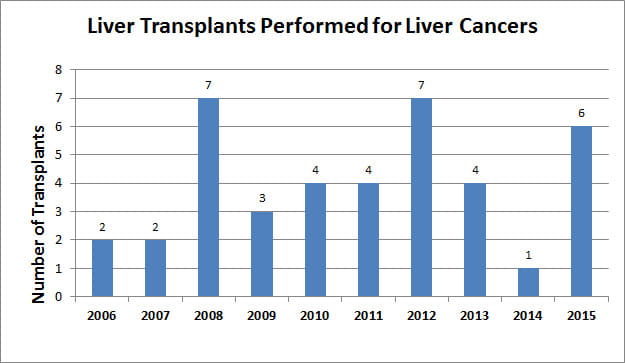
- Number of transplants performed each year
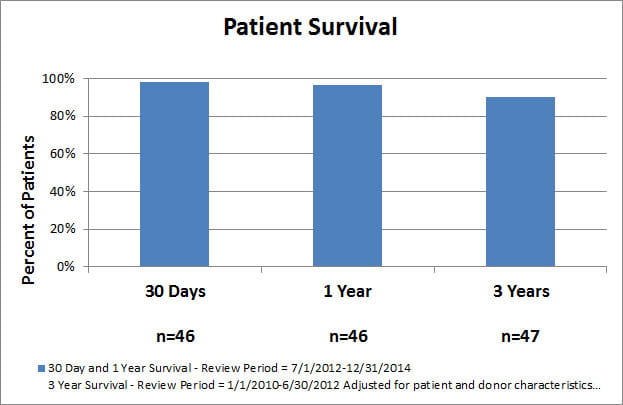
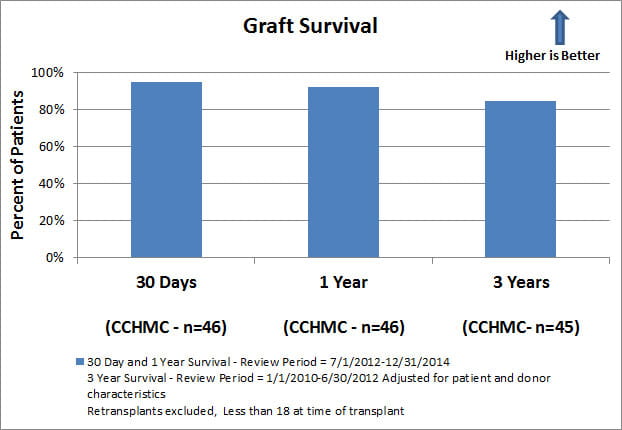
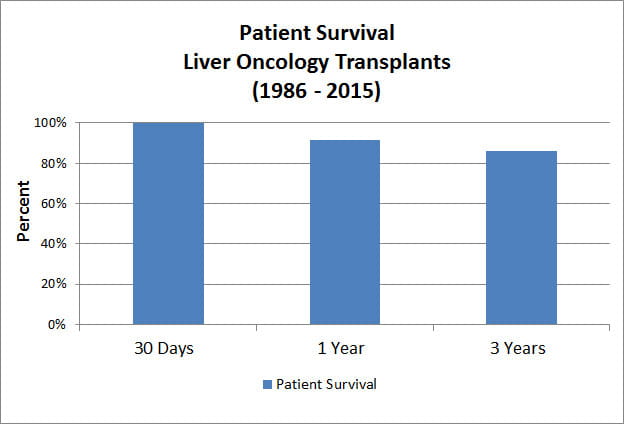
- Overall patient and graft survival following liver transplantation
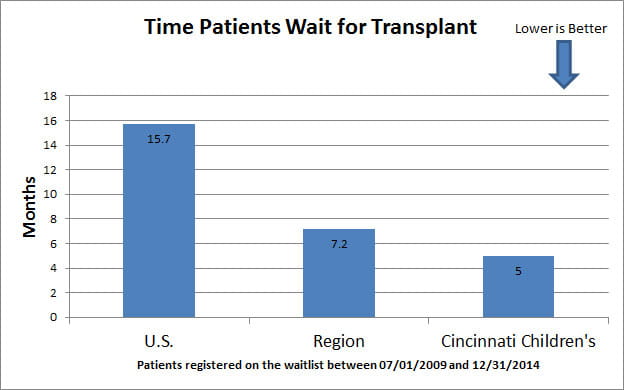
- Mortality while on the wait list and median time to transplant
- Volume and outcomes for pediatric liver tumor transplants
On this page you can learn more about our performance and how we are working to “Change the Outcome” for patients and their families. The statistics are from the Scientific Registry of Transplant Recipients (SRTR), a national database.
Note: “United States / National” data are for illustration only. Based on the unique mix of patients served by a transplant program, and the large difference in numbers between patients transplanted or on the wait list at an individual program and ALL patients transplanted or on the wait list across the country, the numbers and rates may not be directly comparable.