In Memoriam: Jeffrey Robbins, PhD, 1950 – 2022
Post Date: August 22, 2022 | Publish Date:
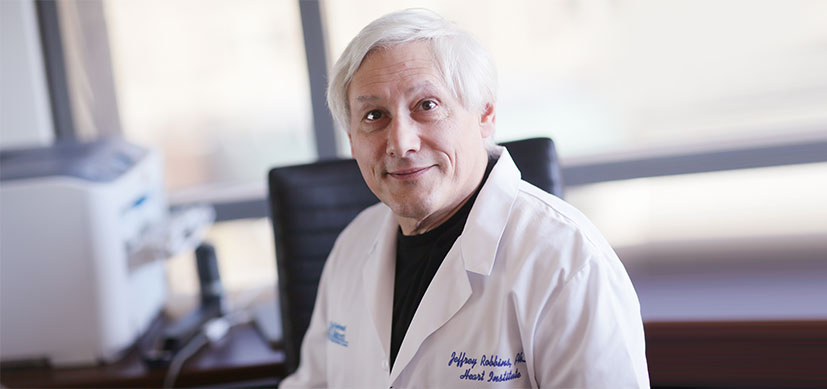
It is with deep sadness that we mourn the loss of Jeffrey Robbins, PhD, professor in the Department of Pediatrics at Cincinnati Children’s, former executive co-director of the Cincinnati Children’s Heart Institute, and former director of the Division of Molecular Cardiovascular Biology, who passed away unexpectedly Aug. 20, 2022. He was 71.
According to Robbins himself, as previously quoted, “When you accomplish what you set out to accomplish, you can look back with some satisfaction.” He certainly had reason to be satisfied when looking back on his career.
Robbins joined Cincinnati Children’s in 1993, and at the time, there was no Division of Molecular Cardiovascular Biology, the Heart Institute wasn’t yet established, and the Division of Sports Medicine within the University of Cincinnati didn’t exist. Robbins was instrumental in the formation of all of these and was a driving force in the study of cardiovascular disease for decades.
Known as a world-renowned researcher and the “father of cardiac transgenesis,” Robbins earned praise for his research in investigating the molecular underpinnings of heart disease and the genetic basis of hypertrophic cardiomyopathy. He conducted pioneering work in generating tissue-specific promoters and gene-targeting approaches for the heart, and his contributions changed the way that basic cardiovascular research is done.
Robbins established one of the most productive laboratories at Cincinnati Children’s, which was the first-ever to isolate genes encoding the major muscle proteins, and the first to ablate a major cardiac contractile protein and show its compensatory effects.
His work led to the development of reagents that have helped scientists understand the actions of proteins responsible for human cardiac disease and design effective therapies. Robbins’ research advanced our understanding of both normal and disease-causing cardiac proteins. Thousands of other investigators have leveraged his data and reagents to advance their own research.
During his time at Cincinnati Children’s, he served as director of the Division of Molecular Cardiovascular Biology, associate chair of the Cincinnati Children’s Research Foundation, and executive co-director of the Heart Institute for 10 years until his retirement in 2019.
Robbins elevated the Heart Institute’s international profile to what it is today. In his role as executive co-director, Robbins represented the research side of the Heart Institute, working closely with Andrew Redington, MD, and the late James Tweddell, MD, helping to guide the team’s path and always with a focus on improving patient care.
His long-time colleague, Jeffery Molkentin, PhD, who now serves as the Heart Institute’s executive co-director and also director of the Division of Molecular Cardiovascular Biology, reflected on the impact that Robbins had at Cincinnati Children’s. “Jeff Robbins founded the Division of Molecular Cardiovascular Biology almost 30 years ago, which led to a long legacy of successful research faculty recruitment and development,” he said.
Robbins also contributed substantially to the success of the entire Cincinnati Children’s Research Foundation, where he was a tireless advocate for research.
“In addition to founding the clinical Sports Medicine program and the Heart Institute at Cincinnati Children’s, he was also one of the prime forces underlying the expansion and tremendous success of the entire Research Foundation over the last 25 years,” Molkentin added. “Jeff was a true visionary in research and program building here, as well as an outstanding mentor and world-renowned heart researcher.”
Over the course of his 50-year career, Robbins published more than 250 peer-reviewed scientific articles and his work has earned some of the most prestigious research awards given by the American Heart Association, the International Society for Heart Research, the University of Cincinnati College of Medicine, and Cincinnati Children’s. These included the American Heart Association’s Research Achievement Award; the International Society for Heart Research’s Distinguished Research Achievement Award; the prestigious Louis and Artur Lucian Award for Research in Circulatory Diseases; the University of Cincinnati’s Rieveschel Award and the Drake Medal; and the William Cooper Procter Medallion, which is the highest award given by Cincinnati Children’s, the first recipient being Albert Sabin in 1960.
“Dr. Robbins was a special leader,” said Tina Cheng, MD, MPH, director of the Cincinnati Children’s Research Foundation, chief medical officer of Cincinnati Children’s, and the Chair of Pediatrics at the University of Cincinnati College of Medicine. “Few people have received both the Drake Medal, the highest honor of the UC College of Medicine, and the William Cooper Procter Medallion, the highest honor bestowed by Cincinnati Children’s. His research discoveries have advanced scientific knowledge and touched patients.”
Robbins was a Fellow of the International Society of Heart Research, the American Heart Association and the International Academy of Cardiovascular Sciences. He served on and chaired numerous national research review committees for the National Institutes of Health and the American Heart Association. He also served on numerous editorial boards and was Associate Editor for a number of journals, including as Cardiovascular Section Editor for the Annual Review of Physiology for 10 years and as Senior Associate Editor for Circulation Research, which is the premier basic science journal for cardiovascular science.
He has mentored more than 30 academic scientists who regard him as the “father of their careers.”
“Jeff recruited me here in 1997, and as a mentor, he had the single greatest impact on my career as a scientist,” Molkentin noted. “We feel his loss deeply and extend our heartfelt condolences to his family.”
Robbins is survived by his wife Roz, his two sons, Stuart and Andrew, and his brother, Scott.
MEMORIAL INFORMATION
Cincinnati Children’s will host a Celebration of Life for Dr. Robbins on Monday, Aug. 29, 2022. The event is by invitation only. Because of COVID-19 safety protocols at the hospital, Cincinnati Children’s has reached the maximum room capacity permitted and cannot accept walk-ins. For additional details, please contact Cara Goyette at Cara.Goyette@cchmc.org.
To share a quote or photo for this event, please contact Carolyn Lipchik at Carolyn.Lipchik@cchmc.org.
Many colleagues, friends, and loved ones have asked how they can honor Dr. Robbins’ legacy. His family requests that donations be directed to Cincinnati Children’s Heart Institute. Click here to be directed to the Cincinnati Children’s donation site. Please check the “Dedicate my donation in honor or memory of someone” box and follow the prompts.
READ MORE ABOUT DR. ROBBINS’ WORK
- 2010 interview with Circulation Research, the journal of the American Heart Association
- Faculty Awards Tribute to Dr. Robbins
- International Academy of Cardiovascular Sciences Medal of Merit Recipient
- Robbins Receives Procter Medallion (2017)
- Robbins Retires, Molkentin Named Director of Molecular Cardiovascular Biology (2019)