Crohn's Disease Treatment
There is no cure for Crohn's disease, but treatment can help control the disease. The treatment depends upon many things:
- Location of the disease
- Problems that the disease may be causing
- How the patient responds to treatment
- The amount of inflammation that is present
The goal of the treatment is to:
- Control symptoms and prevent complications of Crohn’s Disease
- Correct problems the patient may be having with nutrition
- Help keep the disease in remission
- Improve the quality of life
When the disease is under control, treatment is used to keep the symptoms from coming back (a "flare"). Treatment may include:
Medication
Many different types of drugs are used to treat Crohn's disease.
- Anti-inflammatory drugs (aminosalicylates or 5-ASA drugs) are usually used to treat mild to medium symptoms. Some examples are Asacol HD, Pentasa, Lialda, Apriso and Colazal.
- Corticosteroids, such as prednisone, help to put a patient with medium to severe symptoms into remission. These drugs are not good to use for a long time because of side effects.
- Drugs that suppress or quiet the immune system (immunomodulators) are used in moderate to severe Crohn's disease to help patients stay in remission. Some examples are Imuran (azathioprine), purinethol (6-MP) and methotrexate.
- Antibiotics may also be used to treat bacteria in the small intestine that can keep the inflammation going. Some examples are Flagyl (metronidazole), Cipro (ciprofloxacin) and Rifaxamin.
- Biologics are newer drugs approved by the U.S. Food and Drug Administration for treating moderate to severe Crohn's disease that does not respond to the other medications. These medicines are given through a vein (intravenously) or as an injection.
- JAK Inhibitors suppress the immune system to help control the inflammatory process.
- Enteral therapy provides nutrition as a formula rather than eating a regular diet. Enteral therapy has been shown to be effective in treating Crohn’s disease in some patients. There are no side effects to enteral therapy.
Vitamin supplements
Good nutrition is an important part of treating Crohn's disease. No special diet has been proven to be the best for preventing or treating Crohn's disease. Some patients find that symptoms are worse when they have milk, alcohol, hot spices or food containing fiber. Nutritional supplements or special high-calorie liquid formulas are sometimes suggested, especially for children with poor growth. Vitamin levels, such as vitamin D and iron, are checked regularly, and vitamin supplements may be ordered by the doctor.
Surgery
When medication is not able to control the disease or when there are other problems (such as a tight area or hole in the bowel), surgery is needed. Surgery may make symptoms better, but it will not cure Crohn's disease, as the disease can come back. Get as much information as you can about surgery from your doctors, nurses and other patients before making your decision about surgery.
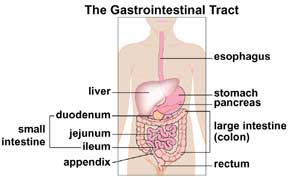
- Bowel resection: When a surgeon removes a section of the intestine damaged by Crohn’s disease or contains a fistula. A fistula occurs when a sore or ulcer in the intestinal tract tunnels through the intestine to surrounding tissue. When a fistula becomes infected, it can create a pocket of pus called an abscess. Fistulas and abscesses are common complications of Crohn’s disease. They can occur within the intestine or in the anus. Medicine can sometimes bring these conditions under control, but if not, the patient may need surgery.
- Anastomosis: When a surgeon removes the diseased part of the intestine and joins the two ends of the healthy bowel together.
- Ostomy: In some patients, it may not be possible to join the two ends of the intestine together. In this case, the surgeon creates a small opening in the front of the abdominal wall. Then the tip of the bowel is brought to the skin's surface. The surgically created opening is called an ostomy. The actual end of the bowel that can be seen protruding through the abdominal wall is called a stoma. Waste leaves the body through the stoma and goes into a bag worn over the opening. Patients who undergo this procedure can live normal, active lives.
In rare cases, patients may need to have their intestine surgically removed. This is called a colectomy. In most situations, the surgeon is able to create an internal pathway for stool to pass, which means your child will not need a colostomy bag.