What is Ulcerative Colitis?
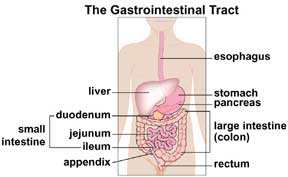
Ulcerative colitis is one of the illnesses known as inflammatory bowel disease (IBD). In ulcerative colitis, the inner lining of the large intestine or bowel (colon) and the rectum become inflamed (irritated or raw and swollen). The colon becomes ulcerated, causing bleeding.
Ulcerative colitis can affect the entire colon, but it is usually in the rectum and the lower part of the colon. Swelling from ulcerative colitis can make the colon empty often, which causes diarrhea.
About 1.4 million Americans have inflammatory bowel disease. IBD is more common in Caucasians. People of all age groups can get ulcerative colitis, but it usually begins between the ages of 15 and 30. Ulcerative colitis affects males and females equally.
Ulcerative Colitis Causes
There is no known cause for ulcerative colitis, but there are many theories about its cause. One theory is that the body's immune system (fights off infection) reacts to a virus or bacteria. This reaction cannot stop and causes chronic (ongoing) swelling in the intestine.
It has been proven that people with ulcerative colitis have problems with their immune system. It is not known if these problems are a cause of the disease or a result of the disease. There is little evidence that ulcerative colitis is caused by emotional distress or allergy to certain foods.
Ulcerative Colitis Symptoms
The most common symptoms of ulcerative colitis are stomach pain and bloody diarrhea (loose bowel movements). Other symptoms that can occur include:
- Rectal bleeding (blood in bowel movements)
- Fatigue (tiredness)
- Loss of appetite
- Weight loss
- Skin problems
- Joint pain
Ulcerative Colitis Diagnosis
A complete medical history and physical examination along with medical tests are used to diagnose ulcerative colitis. The main goal of the tests is to make sure that the disease is ulcerative colitis and not some other kind of disease that causes diarrhea.
Testing for ulcerative colitis includes the following:
- Blood tests to check for anemia (low red blood cell count), which can mean bleeding in the colon or rectum. They can also show if there is an increased number of white blood cells, which might mean that there is swelling somewhere in the body.
- Stool cultures tell if there is an infection by a parasite, virus or bacteria. Stool can also be tested for hidden blood that is not seen on the stool.
- Sigmoidoscopy is a test using a flexible tube with a light and camera lens at the end that is put into the rectum and lower colon (sigmoid colon). It lets the doctor see swelling in the lining of the rectum and lower colon.
- Colonoscopy is a test that uses a long, flexible tube with a light and camera lens at the end. This allows the doctor to examine the lining of the entire colon.
- Biopsy is a tissue sample that is taken for examination and testing in a laboratory. In ulcerative colitis, a biopsy (a small piece of tissue from the lining of the large bowel) is usually done during a sigmoidoscopy or colonoscopy.
- Upper gastrointestinal / GI series is a procedure that examines the stomach and small intestine. Barium is swallowed and then followed through the intestine with an X-ray.
- CT (Computed Tomography) Scan is a CAT scan which uses X-ray to take pictures of the inside of the body. This scan allows the doctors to look at the entire bowel for thickening or inflammation.
- MRI (Magnetic Resonance Imaging) takes pictures of the entire body but does not use radiation. This scan also allows the doctors to look at the entire bowel for thickening or swelling.
Ulcerative Colitis Treatment
Treatment for ulcerative colitis is different from one child to another. What helps one patient may not help another. Treatment for ulcerative colitis depends upon many things:
- Health of the child
- How much of the colon is inflamed
- Ability of the child to take certain medicines or undergo certain procedures
The goal of treatment is to:
- Control symptoms
- Put the disease into remission (making the disease inactive)
- Help keep the disease in remission
- Improve the quality of life
Some patients go into remission (the symptoms of ulcerative colitis go away). However, it is not uncommon for the symptoms to come back (a "flare").
Medication
Several different types of medicines may be used to help control the symptoms of ulcerative colitis. Each helps decrease the swelling in the lining of the colon.
Anti-inflammatory drugs (aminosalicylates or 5-ASA drugs) are usually used to treat mild to medium symptoms. Some examples are Asacol HD, Pentasa, Lialda, Apriso and Colazal.
Corticosteroids, such as prednisone, help to put a patient with medium to severe symptoms into remission. These drugs are not good to use for a long time because of side effects.
Drugs that suppress or quiet the immune system (immunomodulators) are used in medium to severe ulcerative colitis to help patients stay in remission. Some examples are Imuran (azathioprine), purinethol (6-MP) and methotrexate.
Antibiotics may also be used to treat bacteria in the small intestine that can keep the inflammation going. Some examples are Flagyl (metronidazole), Cipro (ciprofloxacin) and Rifaxamin.
Biologics are a newer drug approved by the US Food and Drug Administration for treating medium to severe ulcerative colitis that does not respond to the other medications. This medicine is given through a vein (intravenously) or as an injection.
Surgery
Seventy to 80 percent of children with ulcerative colitis respond well to medicine and a personalized nutrition plan. The rest may require surgery to relieve their symptoms. The most common type of surgery is called “laparoscopic total proctocolectomy with J-pouch reconstruction.”
- Laparoscopic means that the surgery is minimally invasive − the surgeon makes small incisions in the abdomen, not a large, open incision.
- Total proctocolectomy means that the surgeon completely removes the diseased colon.
- J-pouch reconstruction means that the surgeon uses a small section of the small intestine to create a “J” shaped reservoir, or pouch. This pouch, which remains inside the body, allows the body to store and pass stool through the rectum.
Most patients who undergo laparoscopic total proctocolectomy with J-pouch reconstruction have two separate surgeries. In the first, the surgeon creates a temporary ileostomy, or opening in the abdomen. The surgeon will pass the end of the small intestine through this opening, and feces will collect in a bag outside your child’s body. This gives the J-pouch area time to heal.
Two or three months later, the surgeon will perform a second surgery to remove the temporary ileostomy and “reconnect” the small intestine to the rectum. This allows the child to again have bowel movements in the regular manner.
Laparoscopic total proctocolectomy with J-pouch reconstruction is considered major surgery. Since it involves removing the colon, where ulcerative colitis “lives,” this surgery essentially provides a cure for ulcerative colitis. Patients can live normal and active lives after surgery.
Additional Resources
Watch a Video
In a film created by Jesse Dylan, care providers participating in ImproveCareNow discuss how the program's collaborative approach is improving the health of children with Crohn’s disease and ulcerative colitis.



