What is an Alpha-1 Antitrypsin Deficiency (AATD)?
Alpha-1 antitrypsin (ān'tē-trĭp'sĭn) deficiency (AATD) is a disease that is passed down from parents to children. It can cause liver and lung disease. The liver makes a protein called alpha-1 antitrypsin that goes into the bloodstream. This protein protects the lungs and allows them to work normally. If there is not enough alpha-1 antitrypsin available in the body, it is called alpha-1 antitrypsin deficiency (AATD).
AATD is the most common genetic cause of liver disease in children. It is the most common genetic disease that leads to liver transplant in children.
Causes of Alpha-1 Antitrypsin Deficiency
Alpha-1 antitrypsin is a protein that is made in the liver and then released into the bloodstream. In AATD, the body does not make the correct form of this protein. Our bodies need alpha-1 antitrypsin to protect tissues in the body, particularly the lungs. The lack of this protein in the lungs leads to lung disease during adult years. At the same time, the build-up of the abnormal protein in the liver leads to liver disease. About 10% of patients with the severe form of AATD have liver disease that eventually requires a liver transplant.
AATD is an inherited condition and does not appear unless a person receives the same defective gene from both parents. If both parents carry an abnormal gene for AATD there is:
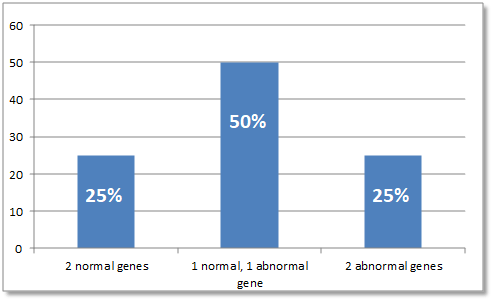
- A 25% chance their child will have the disease
- A 50% chance their child will receive one abnormal gene from one of the parents, which means the child will not show symptoms of the disorder but is a "carrier"
- A 25% chance their child will receive both normal genes, one from each parent, and will be unaffected
It is important to recognize that the severity of the liver and lung disease linked with AATD can vary greatly. Many people with AATD may have no or minimal liver involvement.
Signs and Symptoms
- Jaundice (or yellowing of the skin and eyes) that does not resolve
- Dark urine or pale stools
- Itching of the skin
- Enlarged liver
- Bleeding
- Fluid build-up in the belly (called ascites)
- Trouble eating
- Poor growth or failure to thrive
- Elevated liver enzyme levels
Other children may not show signs of this condition until early childhood. First signs at this age may include:
- Easily tired
- Loss of appetite
- Jaundice
- Fluid build-up in the belly (called ascites)
- Severe itching of the skin
- Panniculitis (rare form of skin disease that causes the skin to harden and form lumps)
- Elevated liver enzyme levels
- Enlargement of the liver or spleen
Diagnosis of Alpha-1 Antitrypsin Deficiency
AATD is diagnosed with a simple blood test that measures the type of alpha-1 antitrypsin found in the blood. This test can tell whether a person has AATD or is a carrier. The blood test can be done soon after a baby is born if there is a family history of the deficiency. A test also is available to check if a baby in the womb has the condition.
Liver disease from AATD is diagnosed through a physical exam and abnormal changes found in the blood. A doctor can tell by feel during a physical exam if something is not normal. Tests, such as an ultrasound of the liver and spleen and a liver biopsy, can help confirm the diagnosis.
If bilirubin (a liquid produced in the liver that removes toxins from the body and helps break down fat in food) levels are higher than normal, it may be a sign of AATD. Increased levels of certain enzymes and abnormal ratios of certain proteins may also indicate liver disease.
Treatment for Alpha-1 Antitrypsin Deficiency
Alpha-1 antitrypsin deficiency affects children differently. One child may not show any signs of liver disease and another child may be seriously affected. Overall, only a small percentage of children develop liver disease related to AATD.
There is no cure for AATD. If severe liver disease develops, a liver transplant is currently the only option available for survival. The goal of treatment is to relieve the symptoms.
- Medicine may be given for severe itching.
- Diuretics (medicines that help remove excess fluid in the body) may be used to help reduce the buildup of fluid in the belly.
- A healthy diet and vitamin supplements can provide needed nutrients and may increase overall health.
- Vitamin/nutrition supplements may increase the effectiveness of the digestive process and increase energy levels.
Transplantation results in a cure of AATD. If a transplant is the best treatment option, the doctor and the other members of the patient care team focus on preventing complications. They will treat symptoms while your child waits for a donated liver. A liver transplant totally replaces the abnormal liver cells that produce the abnormal deficiency and corrects the protein abnormality.
It is critical for a child with AATD to avoid smoking or being exposed to second-hand smoke.
Long-Term Outlook
There is good chance of avoiding liver disease since only about 10% of children with alpha-1-antitrypsin deficiency develop significant liver disease. Liver transplants have been effective in reversing the symptoms of liver failure due to alpha-1 antitrypsin deficiency.



