Cracking the Code of a Brain Cancer That Keeps Coming Back
Cracking the Code of a Brain Cancer That Keeps Coming Back
Sonic Hedgehog Medulloblastoma Can Turn into a Stubborn Killer of Children
Thursday, August 29, 2019
One of the most common brain cancers in children, Sonic Hedgehog (SHH) medulloblastoma, also is one of the more survivable for most kids. Unfortunately, for a subset of patients the cancer resists treatment and relapses with a vengeance to then turn deadly.
Researchers at Cincinnati Children’s Hospital Medical Center used a powerful new computer-assisted technology called single-cell transcriptomics that measures thousands of individual cells simultaneously to map cell types and molecular cascades that drive the growth of SHH-medulloblastoma. In a study published Aug. 29 by the journal Cancer Cell, the scientists report they discovered new treatment strategies for the disease that may help patients fight a recurrent cancer.
Scientists used direct genetic manipulation to block genetic and molecular cascades they discovered in SHH-medulloblastoma tumors. The genetic-molecular block stopped the cancer growth and prevented relapse in tumor-forming laboratory mice, according Q. Richard Lu, PhD, a senior study investigator and scientific director of the Brain Tumor Center at Cincinnati Children’s.
“Medulloblastoma is driven by a diverse group of cell types and molecular pathways that haven’t been understood very well,” said Lu. “But after identifying the molecular triggers and potential cells of origin for tumor initiation and recurrence, we determined from further testing that there are existing small molecule inhibitors that can target the oncogenic cascade pathways that cause SHH tumor initiation and recurrence.”
Cells of Origin Revealed
The researchers developed their new data by subjecting SHH-medulloblastoma tumors in lab animals at various stages of tumor growth to single-cell transcriptomic analysis. The technique generated an extensive dataset that identifies the complete set of transcribed DNA sequences in every single cancer cell. The scan revealed that immature oligodendrocyte progenitor cells in the brain—which can assume stem-cell-like qualities—grow out of control to form medulloblastoma tumors and the molecular cascade that fuels recurring brain cancer.
Although additional preclinical research is needed before clinical testing can be proposed for patients, the current study points to several molecular targets that respond to combined treatment with existing drugs, according to study co-lead author Xuelian He, MD, PhD, a former member of the Lu laboratory and now at Boston Children’s Hospital. Combination therapies allow lower drug doses and improved drug tolerability for patients while achieving a certain level of therapeutic efficacy.
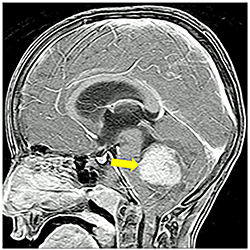
One treatment target proposed by the study is the HIPPO-YAP/TAZ molecular pathway, which can be targeted with an FDA-approved drug already in use for cancer treatment. The pathway is normally responsible for helping control programs that turn cell growth on and off to ensure the body’s tissues and organs are accurately shaped and sized. In SHH-medulloblastoma the pathway becomes overactive. This prompts cells to expand rapidly and grow out of control near the lower central rear of the brain, which mainly controls balance and coordination.
The other potential target is the MYCN/AURORA kinase molecular pathway, which is important in regulating accurate cell structure. In SHH-medulloblastoma, the pathway is overactive and disrupts the formation of cells that otherwise would be structured and function normally. Instead, the cells transform into cancer cells.
Prodrug Potential
Lu said his research collaborators are also working together on a prodrug that will target another molecular cascade related to OLIG2, a protein and transcription factor that is an important regulator in the development of oligodendrocyte cells and motor neurons in the central nervous system. A prodrug is a compound designed as an inactive biological compound that doesn’t turn on and metabolize into a specific, active drug until it reaches the appropriate part of the body.
Molecular testing shows that OLIG2is often elevated in the early stage and treatment-resistant SHH-medulloblastomas. When OLIG2 is overexpressed its energies turn towards forming cancer cells.
Because the preclinical findings in the current study were obtained with human cell cultures and mouse laboratory models, the data will have to be rigorously tested and verified by additional research before clinical testing can be proposed, according to the authors.
Funding support for the research came from the National Institutes of Health (R01 NS078092 and R01 NS075243).
Contact Information
Nick Miller
513-803-6035
nicholas.miller@cchmc.org