Elisa Boscolo, PhD
- Member, Division of Experimental Hematology & Cancer Biology
- Associate Professor, UC Department of Pediatrics
About
Biography
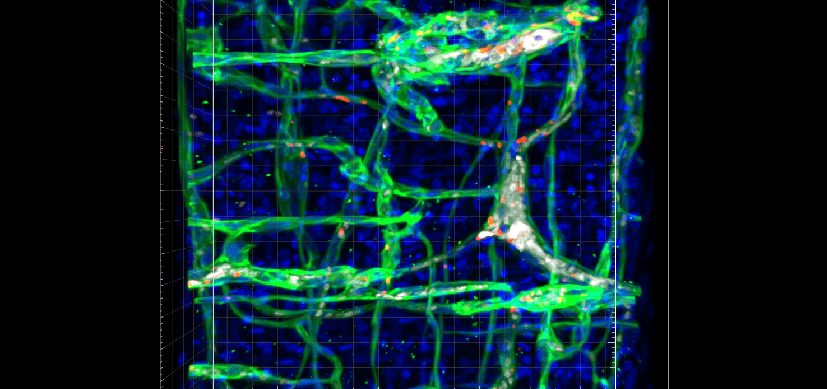
My research focuses on vascular biology. Specifically, I work to deepen the understanding of the cellular and molecular mechanisms underlying vascular anomalies which are pathologies affecting the development of the vascular system. My research helps develop and expand the use of faithful murine models, which provide a solid base for translational research aimed at identifying targeted therapeutic approaches for affected patients.
I joined the Cincinnati Children’s team in 2014, and in 2015 our research team devised a murine model of venous malformation based on the TIE2 mutation identified in patients. Our work showed that the mTOR inhibitor rapamycin (Sirolimus) effectively prevented lesion growth within the murine model. In collaboration with Drs. Miikka Vikkula and Laurence Boon, we then determined its efficacy in a subset of patients enrolled in a pilot clinical trial.
Next, we demonstrated the synergistic effects of ABL kinase inhibition in combination with rapamycin which caused murine venous malformations to regress. Mechanistically, this drug combination enhanced AKT inhibition compared to monotherapy, while also reducing PLCγ/MAPK activity.
The strength of my research program at Cincinnati Children’s is the use of patient-derived biopsies from which we isolate and characterize vascular cells. The patient-derived material is crucial to identify activated signaling pathways, establish murine models of vascular anomalies and test targeted treatments in our pre-clinical studies. Our goal is to determine the pathological mechanisms involved in abnormal blood vessel formation and expansion and to devise strategies to target them in patients.
This unique field of study has allowed me to establish extended collaborations with clinicians and clinician-scientists who are world experts in the field of vascular anomalies. Our working together is a cornerstone for the investigation and identification of novel efficacious therapeutic strategies for children affected by vascular tumors or malformations.
I have been honored by the International Society for the Study of Vascular Anomalies (ISSVA) with the John Mulliken Award and Best Scientific Paper in 2014. I have also received the 2020 Werner Risau Early Career Investigator Award in Vascular Biology from the American Heart Association.
BS: Molecular Biology, University of Padua, Padova, Italy,
PhD: Tissue Engineering, University of Padua, Padova, Italy,
Fellowship: Vascular Biology, Boston Children’s Hospital, Harvard Medical School, Cambridge, MA,
Services and Specialties
Interests
Vascular anomalies; endothelial cell biology; mTOR signaling.
Research Areas
Publications
Semaphorin 3A and 3F Promote Lumen Expansion in TIE2-Mutated Venous Malformation. Arteriosclerosis, Thrombosis, and Vascular Biology. 2025; 45(12):2243-2260.
Capillary malformations. Journal of Clinical Investigation. 2024; 134(8).
MEK inhibition reduced vascular tumor growth and coagulopathy in a mouse model with hyperactive GNAQ. Nature Communications. 2023; 14(1):1929.
Constitutively active PIK3CA mutations are expressed by lymphatic and vascular endothelial cells in capillary lymphatic venous malformation. Angiogenesis. 2020; 23(3):425-442.
Constitutive Active Mutant TIE2 Induces Enlarged Vascular Lumen Formation with Loss of Apico-basal Polarity and Pericyte Recruitment. Scientific Reports. 2019; 9(1):12352.
Ponatinib Combined With Rapamycin Causes Regression of Murine Venous Malformation. Arteriosclerosis, Thrombosis, and Vascular Biology. 2019; 39(3):496-512.
A xenograft model for venous malformation. Angiogenesis. 2018; 21(4):725-735.
Rapamycin improves TIE2-mutated venous malformation in murine model and human subjects. Journal of Clinical Investigation. 2015; 125(9):3491-3504.
AKT hyper-phosphorylation associated with PI3K mutations in lymphatic endothelial cells from a patient with lymphatic malformation. Angiogenesis. 2015; 18(2):151-162.
From the Blog
New Mouse Model Enables Discovery of Potential Treatment for Rare Vascular Tumors—and Beyond
Elisa Boscolo, PhD4/24/2023