Carole Lannon, MD, MPH
- Senior Faculty Lead, Learning Networks Core, Anderson Center for Health Systems Excellence
- Professor, UC Department of Pediatrics
About
Biography
Identifiable gaps in health outcomes piqued my research interests. I now work with patients, families, clinicians and researchers to improve care and outcomes for children and families using learning health networks. These networks, used for improvement and research, can accelerate population health outcomes at scale.
Working with my colleagues, we determined that the Learning Health Network model reliably reproduces results at scale. This model has already been effective for networks focusing on chronic conditions, rare diseases, safety and population health.
I joined Cincinnati Children’s Hospital Medical Center in 2006 to research learning health networks, collaborative science, quality improvement, and patient and family partnerships. All the outcomes I’ve achieved have come as a direct result of partnering with others.
Patient and family care has been truly transformative for me. The experience has helped me dramatically improve our learning health network outcomes. Additionally, improvement science has helped me understand the value of standardization, since the reliability of processes and results supports a platform for innovation.
As a result of my work, I have been honored with the 2020 Cincinnati Children’s Advocacy Award. I also serve as the senior quality advisor for the American Board of Pediatrics.
MD: University of Minnesota Medical School, Twin Cities, MN, 1982,
Residency: Medicine-Pediatrics, University of North Carolina, Chapel Hill, NC,
Fellowship: Robert Wood Johnson Clinical Scholars Program, University of North Carolina, Chapel Hill, NC,
MPH: Epidemiology, University of North Carolina, Chapel Hill, NC, 1993,
Certifications: Internal Medicine, 1986; Pediatrics, 1988
Research Areas
Publications
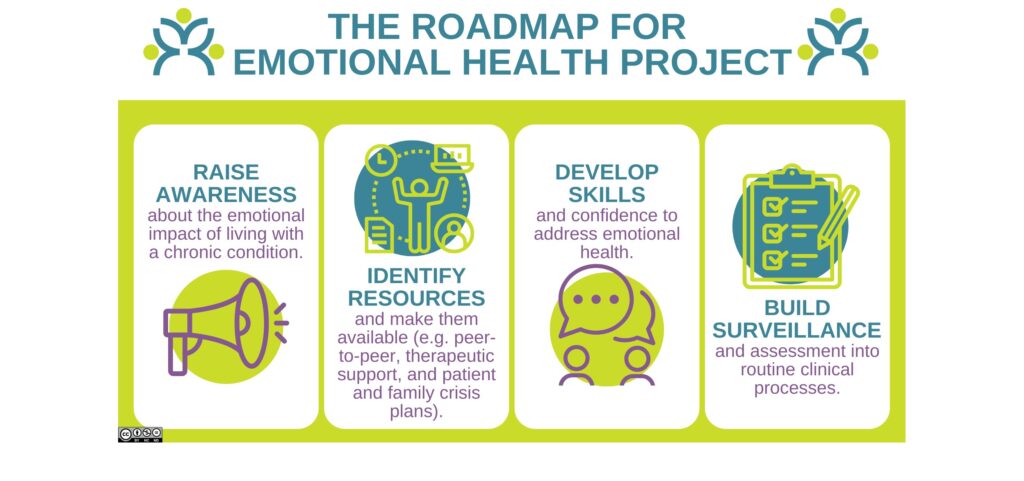
Partnering With Patients and Families on the Roadmap for Emotional Health. Journal of Participatory Research Methods. 2025; 6(4).
Association Between Obesity-Related Health Factors and Patient-Reported Outcomes: Linking Patient-Reported Outcomes to PEDSnet Electronic Health Record Data. Childhood Obesity. 2025; 21(5):438-448.
Transitioning medically complex infants home: lessons learned from quality improvement efforts. Journal of Perinatology. 2025; 45(3):404-410.
Increasing Capacity to Address Emotional Health for Children with Chronic Conditions and their Families: Roles for Pediatric Psychologists. Translational Behavioral Medicine. 2025; 15(1).
Perinatal Naloxone Care Practices: Survey Results From Persons With OUD and Providers. Journal of Addiction Medicine. 2025; 19(1):62-67.
Supporting the Well-Being of Children and Youth With Special Health Care Needs: NASEM Proceedings. Pediatrics. 2024; 154(6).
Integrating education for clinical practice change. Clinical Teacher. 2024; 21(4):e13753.
The NEONATE score predicts freedom from interstage mortality or transplant in a modern cohort. Cardiology in the Young. 2024; 34(5):981-988.
Risk Factors for Death or Transplant After Stage 2 Palliation for Single Ventricle Heart Disease. JACC: Advances. 2024; 3(5):100934.
Patient-Reported Outcomes to Describe Global Health and Family Relationships in Pediatric Weight Management. Childhood Obesity. 2024; 20(1):1-10.
From the Blog
A Shared Responsibility for Emotional Health
Carole Lannon, MD, MPH, Lori E. Crosby, PsyD9/16/2025
Smoothing the Transition from NICU to Home
Carole Lannon, MD, MPH, Dan Benscoter, DO4/22/2025
National Academies Address Well-Being of Youth with Special Health Care Needs
Carole Lannon, MD, MPH, Thomas F. Boat, MD11/27/2024
Successfully Integrating Emotional Health Assessments into Pediatric Care
Carole Lannon, MD, MPH11/11/2024
Pediatric Trainees Use ‘Roadmap Project’ Tools to Address Emotional Health
Carole Lannon, MD, MPH, Lori Herbst, MD ...9/5/2024
Being Black with a Chronic Condition
Carole Lannon, MD, MPH, Christine L. Schuler, MD, MPH2/21/2023