What is a Nasogastric Tube Feeding Using a Feeding Pump?
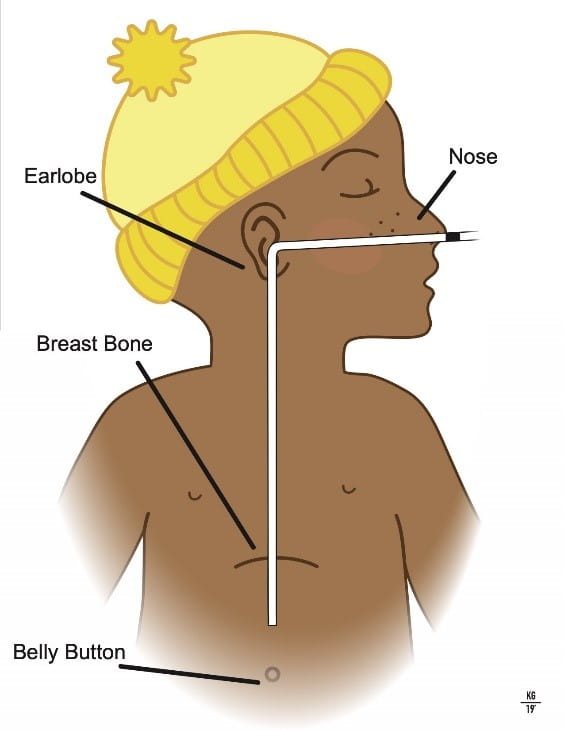 A nasogastric (NG) tube is a thin, soft tube that passes through the nose and into the stomach. The NG tube allows your child get the nutrition, fluid and / or medications that he / she needs. NG tube training sessions must occur for all patients at home with a feeding tube.
A nasogastric (NG) tube is a thin, soft tube that passes through the nose and into the stomach. The NG tube allows your child get the nutrition, fluid and / or medications that he / she needs. NG tube training sessions must occur for all patients at home with a feeding tube.
How Do I Know the NG Tube Is in the Right Place?
-
Wash your hands with soap and water.
-
Check that the NG tube is in the right place:
-
Measure the outside length of the tube and check that this is has not changed. External length = measurement of feeding tube from nostril to base of the hub. OR check the marking on the NG tube, making sure it is right next to the nostril.
AND
-
Connect a 5 – 10 ml syringe to the end of the NG tube and pull back to get stomach contents.
-
Do not return the stomach contents back in the tube.
-
-
-
If you are unable to remove the stomach contents, remove the syringe, close the cover over the end of the tube, and place your child on their left side. After 10 minutes, repeat the attempt to pull back stomach contents into a syringe.
-
If you can remove stomach contents, discard the contents and proceed with “Give a feeding” (listed below).
-
If you are unable to remove stomach contents, remove the NG tube and reinsert tube.
-
How do I give a feeding?
1.Wash your hands with soap and water.
2.Gather the supplies:
- Feeding pump
- Feeding administration bag
- IV pole
- Farrell valve system bag (if ordered by your doctor)
- Formula / breastmilk
- Bottle or container to measure formula / breastmilk
- Small syringe 5-10 ml
- Water
3.Open the feeding administration set and the Farrell bag (as ordered for decompression).
- Use a new feeding administration set and Farrell bag every 24 hours.
4.Connect the bags at the “Y” junction on the Farrell bag tubing.
5.Add the formula / breastmilk to the bag.
- Formula / breastmilk that you mix or prepare can be in the bag for four hours.
- Formula that is already prepared and in a box can be in the bag for eight hours.
- If your child is immunocompromised, only 4 hours of milk can be hung at one time.
6.Prime, or fill, the tubing of the feeding administration set with formula / breastmilk.
- Stop the formula / breastmilk just before it reaches the end of the tubing.
- This prevents formula / breastmilk from getting into the grooves on the end of the feeding tube.
7.Put the tubing into the feeding pump.
8.Turn the pump on.
9.Refer to feeding pump instructions for pump programming.
- Set the rate – how fast the feedings are to go in
- Set the dose − how much formula / breastmilk is to be given
10.Check to make sure the NG tube is in the correct place. (see above)
11.Connect the feeding administration set tubing to the feeding tube.
12.Start the feeding pump.
13.When the feeding is finished, turn off the pump, remove the feeding set and flush the NG tube with water.
14.Clean the end of the feeding tube with a toothbrush and warm water.
What Other Things Do I Need to Remember?
- If your child begins to choke or gag during a feeding, stop the feeding pump.
- Re-check tube placement.
- Continue with the feeding when your child is no longer choking or gagging.
- Know that there is a possibility that your child could throw up and the tube could come out of his / her mouth. Remember to remove the tape and then remove the tube from your child’s nose.
- If child's stomach becomes large and round or if he / she have discomfort, stop the feeding and wait one hour.
- If the stomach remains large and round or if your child continues with discomfort after one hour, call your nurse or doctor.
- Never add new formula / breastmilk to formula / breastmilk that is already in the feeding bag. Empty any old formula / breastmilk before adding new formula / breastmilk.
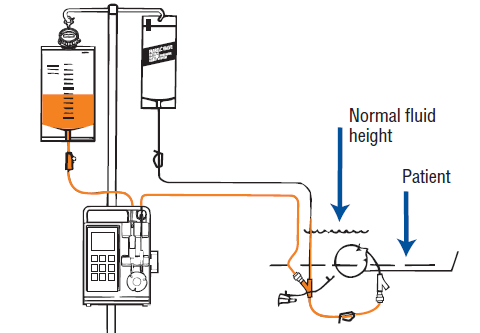
- Keep the “Y” of the administration set / Farrell valve connection at the stomach level.
- Flush the feeding tube before and after giving medications as directed by your provider. This helps to keep the feeding tube from clogging.
- If you remove the NG tube, pinch the feeding tube so that formula does not drip from the tube and get into your child’s lungs.
- If the feeding tube has a stylet (thin wire that goes in the NG tube during placement), save the stylet. You will need to re-insert the stylet when you reinsert the NG tube
- You can re-use the same feeding tube.
- Always check the end of the feeding tube that goes into the stomach for any holes or tears before you replace it.
- It is important to allow your infant or child to have pleasant sensations during feedings: hold during feedings, suck on a pacifier, sit in a high chair, be a part of family meals
- Ask your doctor or nurse about therapy to help improve oral skills.
What Do I Do If Formula / Breastmilk Backs Up into the Farrell Bag?
If formula / breastmilk backs up into the Farrell bag, this means your child’s stomach cannot handle the feedings or there is a problem with the tubing or the feeding tube.
- First, close the clamp on the Farrell bag.
- Check your child to make sure their stomach is not swollen or bloated.
- Check the feeding tube for kinks.
- Check to make sure the feeding tube is not clogged:
- Disconnect the Farrell tubing from the feeding tube.
- Flush the feeding tube with a small amount of water.
- Drain the formula / breastmilk from the Farrell bag into a cup.
- You need to do this because you cannot control how fast the formula / breastmilk flows.
- Disconnect the Farrell bag tubing and open the clamp.
- Measure the amount of formula / breastmilk not given.
- If child and the feeding tube are OK, raise the Farrell bag higher to avoid having formula / breastmilk back up into the bag.
- If the problem persists, call your provider.
Call Your Doctor or Nurse If:
- Your child is uncomfortable or fussy with feedings.
- Your child vomits or has diarrhea.
- Your child’s stomach is swollen or bloated.