What Are the Types of TAPVR?
Total anomalous pulmonary venous return is classified into different types. This is based on how and where the pulmonary veins drain to the heart:
Supracardiac Total Anomalous Pulmonary Venous Return
The pulmonary veins drain to the right atrium by the superior vena cava. In this type of TAPVR, the pulmonary veins come together behind the heart and then drain upwards to an abnormal “vertical vein.” This vertical vein joins the innominate vein which connects to the right superior vena cava and drains to the right atrium.
Cardiac Total Anomalous Pulmonary Venous Return
The pulmonary veins come together behind the heart. They then drain to the right atrium through the coronary sinus. The coronary sinus is the vein that normally returns blood from the heart muscle itself back to the right atrium after its oxygen has been used. The coronary sinus drains directly into the right atrium.
Infracardiac Total Anomalous Pulmonary Venous Return
The pulmonary veins drain to the right atrium by the hepatic (liver) veins and inferior vena cava. In this type, the pulmonary veins join together behind the heart. They then drain downwards, connecting to the liver's portal vein system. They drain through the vascular bed of the liver and enter the right atrium from the hepatic veins.
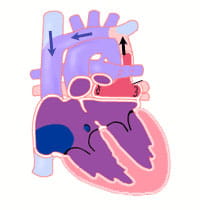
All types of total anomalous pulmonary venous return must have an atrial septal defect (ASD). An ASD is a hole in the wall between the right and left upper chambers of the heart. This hole will allow some of the oxygenated blood that has entered the right atrium from the pulmonary vein to go across to the left atrium and out to the body.
What Problems Are Associated With TAPVR?
Because of the abnormal pulmonary vein connection red (oxygenated) blood returning from the lungs mixes with the blue (lower oxygenated) blood returning from the body.
The left side of the heart (left atrium and left ventricle) is filled only by mixed blood. Because this blood is a mixture of red and blue (oxygenated and deoxygenated) blood, the overall oxygen content is decreased in the blood leaving the heart and going to the body. This is why patients with TAPVR have low oxygen saturations.
If the atrial septal defect (ASD) is small or limits blood flow from the right atrium to the left atrium, then the volume of blood filling the left atrium and left ventricle may be lessened. This can lead to low blood supply to the body and shock.
In some cases of TAPVR, the route of blood from the pulmonary veins back to the heart may have areas of narrowing or obstruction. This obstruction may stop a normal amount of blood return from the pulmonary veins. It may increase the pressure in the veins. Blockage in the pulmonary veins leads to congestion in the lungs (pulmonary edema, or excessive fluid) and pulmonary hypertension (high pressure in the lung vessels).
Patients with obstructed TAPVR are critically ill with severe cyanosis and often have very unstable blood pressure. Surgery may be needed right away for these patients.
Obstructed pulmonary veins commonly occur in the infracardiac type of TAPVR. It can occur with the other anatomic types as well.
What Are the Symptoms of TAPVR?
Patients with obstructed total anomalous pulmonary venous return (TAPVR) are ill soon after birth. These children are severely cyanotic (blue coloring to skin, lips and nails). They also have respiratory problems, rapid breathing, grunting and retractions of the rib cage muscles.
If obstruction to pulmonary venous return is not present, children with TAPVR may not have many symptoms. There may be some fast breathing or trouble breathing. There is often cyanosis. It may be mild and hard to see.
Some children with this more common type of TAPVR are diagnosed when a doctor hears a heart murmur during a physical examination. These children may not be diagnosed for several weeks to months.