Overview
We are actively investigating pediatric sepsis-associated myocardial dysfunction (SAMD), focusing on the response of human induced pluripotent stem cell (iPSC)-derived cardiomyocytes to serum factors from children with septic shock, as well as patterns of susceptibility to SAMD using patient-specific iPSC-cardiomyocytes. In collaboration with the Atreya Laboratory, we are also developing a biorepository of patient-specific iPSCs from children with septic shock to unravel mechanisms of organ dysfunction.
iPSC-Cardiomyocyte Response to Septic Serum
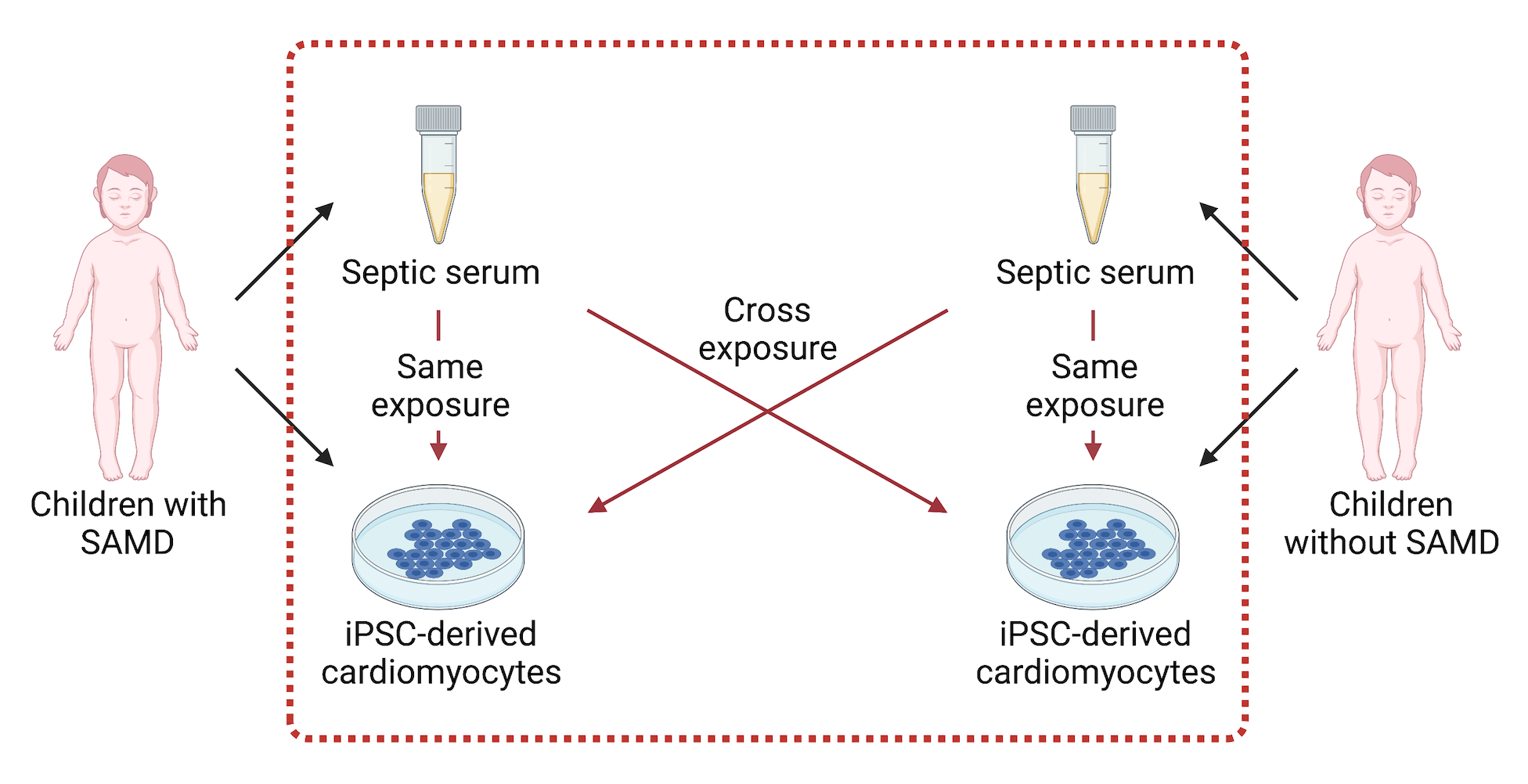
iPSC-derived cardiomyocytes are a renewable platform to study the human cardiomyocyte response to septic serum and specific circulating myocardial depressant factors. We use small molecules to direct iPSCs to differentiate into cardiomyocytes in our laboratory, which spontaneously beat. We have demonstrated that serum from children with SAMD reliably depresses the contractility of iPSC-cardiomyocytes, compared to serum from children with sepsis but no SAMD. To contextualize and better understand the mechanisms driving these changes in contractility, we measure a variety of readouts, including mitochondrial function and changes in gene expression. We have also begun to examine the role of specific cytokines and serum factors in SAMD through modulation of signaling pathways in iPSC-cardiomyocytes.