Improving Outcomes for Infants with Gastroschisis
Gastroschisis is one of the few birth defects increasing in prevalence—based on current estimates, four to five occur per 10,000 live births.
Clinical History and Presentation
Following a routine fetal ultrasound in the second trimester, a 23-year-old expectant mother learned that her unborn son was diagnosed with gastroschisis. Subsequent ultrasound examinations also detected suspected bowel atresia. The mother was referred to the Cincinnati Fetal Center, located at Cincinnati Children’s Hospital Medical Center.
The Fetal Center confirmed the diagnosis of gastroschisis and bowel atresia through an ultrasound and ultrafast fetal MRI. Physicians scheduled the baby’s delivery at Good Samaritan Hospital in Cincinnati to facilitate immediate surgery upon birth. However, the mother went into labor at 34 weeks and delivered the baby boy at her home hospital, three hours away.
Upon delivery, the newborn exhibited gastroschisis and small bowel atresia, with possible vascular compromise to a portion of the bowel. The newborn was stabilized and urgently transferred to the Level IV Neonatal Intensive Care Unit (NICU) at Cincinnati Children’s.
Our Approach
Upon arrival, the infant immediately underwent an exploratory laparotomy with removal of necrotic bowel. Due to concern about the viability of the residual bowel, the remainder of his bowel was placed in a silo and parenteral nutrition was initiated.
Following surgery, a team of neonatologists, surgeons, dietitians, social workers and care coordinators collaborated on the infant’s care. The team conducted daily rounds in the NICU, which allowed for immediate, joint treatment decisions. In addition, the Intestinal Rehabilitation Team—a gastroenterologist, neonatologist, surgeon and dietitian—rounded with the group each week to monitor the child’s feeding tolerance and confer on any nutrition complications.
At the time of the first surgery, only 30 cm of his bowel appeared viable due to necrosis; however, a large amount of inflammatory peel prevented visualization and confirmation. At subsequent surgeries, additional segments of viable bowel became apparent. The complicated nature of the infant’s condition precluded putting him immediately on the gastroschisis nutritional protocol, so parenteral nutrition continued.
Nutritional Protocol
At six weeks, surgeons reconnected his proximal bowel. Despite the return of bowel continuity, the infant had prolonged feeding intolerance with stricture formation. Over the next several months, he underwent multiple surgeries for removal of strictures, as well as a tapering procedure. After bowel reconstruction, our staff managed him as closely as possible with the nutritional protocol set forth by our team of experts.
Once his gastric output fell to <20 ml/kg/day and he began stooling, continuous feeds of breast milk or elemental formula were initiated, advancing by 1 ml/hour each day until he tolerated 5 ml/hour. Advancement then proceeded at a faster rate. After he achieved goal volumes, breast milk or formula was fortified to reach goal caloric intake (generally 120 kcal/kg/day). Finally, the continuous infusion was consolidated to bolus feeding and occasional bottle feeds.
Intestinal Rehabilitation
Once the infant’s acute issues resolved at three months, he was transferred to the gastrointestinal service, where the Intestinal Rehabilitation Team continued following him. To ensure coordination of care, nutritionists from the NICU consulted with the nutritionists on the GI service regarding the nutritional protocol. After a nine-month hospitalization he was discharged to home, where he continued to be fed via G-tube while also receiving parenteral nutrition.
Clinical Outcome and Follow Up
The boy, currently 18 months old, has experienced slow growth, but it is improving. His enteral feedings are increasing while his parenteral nutrition is decreasing. Because he was discharged with a G-tube and was still receiving parenteral nutrition, the Nutrition and Intestinal Care Center at Cincinnati Children’s continues to follow him. During his monthly visits, he also works with speech therapists and occupational therapists to improve his oral feeding skills.
Neonatal nutritionists also support his local pediatrician by providing input on feeding decisions and conferring on nutrition-related medical issues. They work together to encourage normal nutritional developmental milestones, aiming for his nutritional independence.
Discussion
This case is indicative of the potential spectrum of problems that infants with gastroschisis encounter, placing them at risk for poor long-term neurodevelopment, slow growth and gastrointestinal morbidity. Despite these risks, little research has focused on outcomes after initial hospital discharge.
This may be due to its low prevalence (<2,000 infants affected in the U.S. each year) or to a misunderstanding of the known outcomes. Until recently, most providers thought that the care and follow-up of infants with gastroschisis was straightforward and well defined; however, emerging data we have gathered suggest this may not be the case.
Latest Research Efforts for Infants with Gastroschisis
Few randomized trials to evaluate treatment choices for infants with gastroschisis have been performed. Furthermore, outcomes evaluated have not typically extended beyond the perinatal period, making it difficult to treat the condition today and to understand long-term outcomes. We are improving our understanding of the condition through pioneering research of both short- and long-term outcomes.
It is evident that further study is needed to better define long-term outcomes for gastroschisis and to determine and test strategies to optimize outcomes. However, we must define problems before we can solve them.
Short-term Outcomes
To define the problems, we are working to track short-term outcomes for infants born with gastroschisis. We are gathering data, including details about growth and nutrition, to allow us to describe outcomes and identify determinants. Our standard nutritional strategy, including the use of parenteral nutrition, timing of initiation of feeds and content of enteral feeds, is part of this data collection. In addition, we are planning a randomized trial to determine if this nutritional strategy optimizes short-term outcomes.
Long-term Outcomes
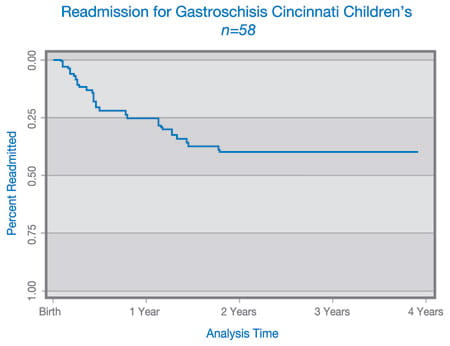
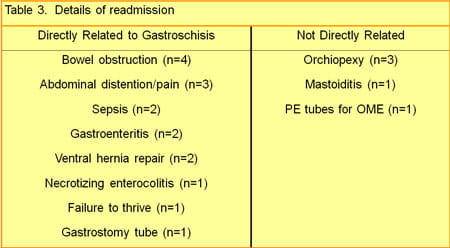
Our second step is to follow all infants with gastroschisis long term. In the past, only infants with significant residual problems were followed long term. We plan to obtain longitudinal growth and formal neurodevelopmental data in addition to monitoring other morbidities, including readmissions and gastrointestinal complications such as constipation, bowel obstruction and malabsorption.
Long-term outcomes can be effectively analyzed by determining associations between neonatal risk factors—mode of delivery, method of surgical repair and use of breast milk as part of an enteral feeding regimen—and important clinical outcomes, including growth, neurodevelopment, and functional bowel disorders (e.g., constipation and diarrhea).