Computational Fluid Dynamics and Airway Research
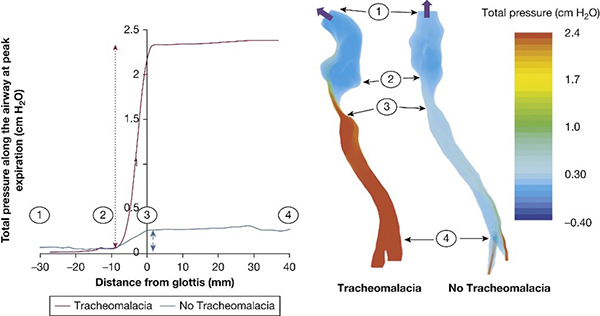
Our research focuses on human airways and how they change in various disease conditions. We research airway behavior in children with obstructive sleep apnea (OSA) and premature babies born with tracheomalacia (TM) and congenital abnormalities. Our goals are to identify how airway problems affect patients’ symptoms, inform, and evaluate surgical and therapeutic interventions, and differentiate the effects of airway abnormalities versus lung disease.
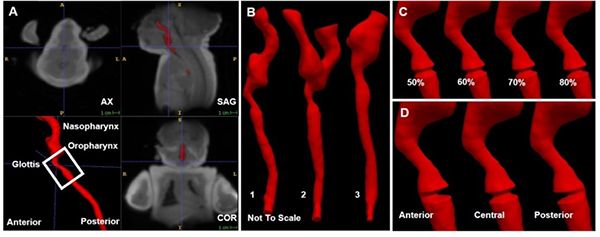
Our researchers have the world's first virtual models of human airways that move realistically base the motion on high-speed magnetic resonance imaging (MRI).
The effects of airway diseases are difficult to measure in patients and deciphering which treatments will be effective. We create virtual models of airways from MRIs. We then use computational fluid dynamics (CFD) to simulate how air flows through the airway. This model shows us where in the airway are regions with high resistance. We can virtually alter the airway to predict how it would change after treatment. We also calculate the effect that treatment would have on airway symptoms. Our goal is to predict the best treatment approach for children with OSA and premature babies with TM.