Scott W. Powers, PhD, ABPP, FAHS
- Pediatric Psychologist, Research, Division of Behavioral Medicine and Clinical Psychology
- Cincinnati Children’s Research Foundation Endowed Chair
Scientific Director, Clinical Research and Trials
Co-Director, Headache Center
Director, Center for Child Behavior and Nutrition Research and Training - Professor, UC Department of Pediatrics
- emily.conner@cchmc.org
- Board Certified
About
Biography
As a pediatric psychologist, as well as a clinical child and adolescent psychologist, I practice evidence-based behavioral medicine. I treat children with migraine and other types of headache.
At Cincinnati Children’s, I am the scientific director of Clinical Research and Trials for the Research Foundation, the co-director of the Headache Center, and the director of the Center for Child Behavior and Nutrition Research and Training.
My research includes clinical trials in the areas of migraine and headache as well as child behavior and nutrition science. Migraine affects 10% of youth today. It’s one of the most common chronic illnesses of childhood and is the second most prevalent disabling condition worldwide. It affects people from childhood throughout most of their lives. My colleagues and I strive to develop the evidence-based treatments of tomorrow while building teams to provide the best care we can today. If youth have improvements in headache occurrence and related disability, then we may change the course of their lives.
Our team has published game-changing clinical trials in prestigious journals, such as the New England Journal of Medicine, the Journal of the American Medical Association (JAMA), JAMA Pediatrics and Pediatrics.
During my career, I am honored to have received both the research and mentoring awards from the Society of Pediatric Psychology, a division of the American Psychological Association.
AB: Wabash College, Crawfordsville, IN, 1985,
MD: Idaho State University, Pocatello, ID, 1987,
PhD: The University of Alabama, Tuscaloosa, AL, 1991,
Residency: Clinical Psychology, Brown University School of Medicine, Providence, RI,
Fellowship: Pediatric Psychology, Brown University School of Medicine / Rhode Island Hospital, Providence, RI,
Certifications: Clinical Psychology, Ohio State Board of Psychology, 1992; American Board of Professional Psychology (ABPP), 2003
Interests
Preschoolers and toddlers; dietary adherence / nutrition and behavior; cystic fibrosis; chronic illness, coping and adherence; pediatric pain; pediatric headache; encopresis.
Services and Specialties
Interests
Clinical trials; migraine/headache; pediatric pain; adherence medicine; nutrition and behavior; cystic fibrosis
Publications
Multimodal Assessment of Medication Adherence Among Youth With Migraine: An Ancillary Study of the CHAMP Trial. Journal of Pediatric Psychology. 2022; 47(4):376-387.
Trajectory of treatment response in the child and adolescent migraine prevention (CHAMP) study: A randomized clinical trial. Cephalalgia. 2022; 42(1):44-52.
Prevalence of Headache Days and Disability 3 Years After Participation in the Childhood and Adolescent Migraine Prevention Medication Trial. JAMA Network Open. 2021; 4(7):e2114712.
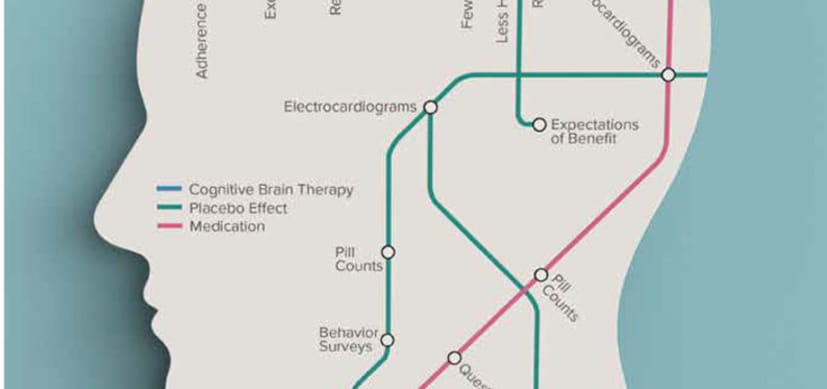
Alterations in Brain Function After Cognitive Behavioral Therapy for Migraine in Children and Adolescents. Headache. 2020; 60(6):1165-1182.
Treatment Adherence in Child and Adolescent Chronic Migraine Patients: Results From the Cognitive-Behavioral Therapy and Amitriptyline Trial. Clinical Journal of Pain. 2017; 33(10):892-898.
Treatment of Pediatric Migraine. New England Journal of Medicine. 2017; 376(14):1388-1389.
The Childhood and Adolescent Migraine Prevention (CHAMP) Study: "What Do We Do Now?". Headache. 2017; 57(2):180-183.
From the Blog
15-Site Trial to Compare Telehealth Cognitive Behavior Therapy Alone and with Medication to Prevent Migraine in Youth
Scott W. Powers, PhD, ABPP, FAHS7/26/2022
How Can CBT Be Expanded Beyond Specialty Headache Centers?
Scott W. Powers, PhD, ABPP, FAHS2/2/2022
Research Reinforces Alternatives to Medication in Migraine Care
Scott W. Powers, PhD, ABPP, FAHS, Andrew D. Hershey, MD, PhD, FAAN, FAHS7/27/2021
Teaming Up to Solve a Headache About Headaches
Scott W. Powers, PhD, ABPP, FAHS, Robert C. Coghill, PhD ...7/3/2019








Patient Ratings and Comments
All patient satisfaction ratings and comments are submitted by actual patients and verified by a leading independent experience management company, Qualtrics. Patient identities are withheld to ensure confidentiality and privacy. Only those providers whose satisfaction surveys are administered through Cincinnati Children’s Hospital Medical Center are displayed. Click here to learn more about our survey