Understanding Eosinophilia
Eosinophilia is having high levels of eosinophils, which are a type of immune cell that is normally present in the blood and certain tissues, including the spleen, lymph nodes and thymus and parts of the gastrointestinal, respiratory and genitourinary tracts.
When the body wants to attack a substance, such as an allergy-triggering food or airborne allergen or a parasite, eosinophils respond by moving into the area and releasing a variety of toxins. (Read more: What is an Eosinophil?) However, when the body produces too many eosinophils, called “eosinophilia”, the eosinophils can cause chronic inflammation resulting in tissue damage.
How Many Eosinophils is Too Many?
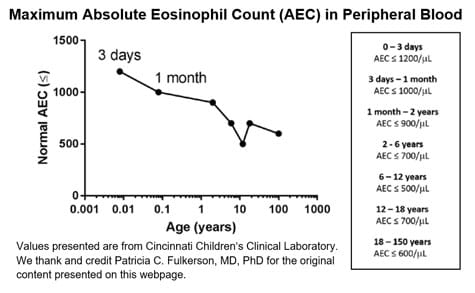
What are “normal” or “above-normal” amounts of eosinophils? Currently, there are no published, established guidelines to answer this question, and the amount of eosinophils will vary by location in the body. However, we know from our clinical laboratory here at Cincinnati Children’s that the maximum absolute eosinophil count (AEC) in the peripheral blood varies by age, with it being higher in younger children.