In Uganda, Rheumatic Heart Disease Research Reaches its GOAL
Published January 2022 | New England Journal of Medicine
The study was dubbed “Gwoko Adunu pa Lutino” (GOAL), meaning “protect the heart of a child.”
Its findings addressed a surprisingly common yet under-researched condition that poses serious long-term risks: rheumatic heart disease.
“The GOAL trial is a stunning example of global collaboration, including investigators from six continents working together to find innovative solutions to reduce the global burden of rheumatic heart disease,” says principal investigator Andrea Beaton, MD.
Rheumatic heart disease is a chronic valvular heart disease caused by rheumatic fever, which develops after an untreated case of strep throat. More than 40.5 million people globally are estimated to be living with rheumatic heart disease, and approximately 306,000 deaths are attributed to it annually.
In the U.S., rheumatic fever and rheumatic heart disease were leading killers of children and young adults in the early 1900s. But widespread use of penicillin after World War II stopped the deaths, and now most cases of strep throat are treated long before serious complications arise.
But in low-resource settings, 85% of children with rheumatic heart disease are diagnosed only after the disease has become well-advanced. This makes medications ineffective and surgical intervention (typically heart valve replacement) less likely to succeed if available at all.
“Imagine people in their 20s coming into the hospital because they’ve had a stroke,” says Emmy Okello, MD, chief of cardiology at the Uganda Heart Institute and co-principal investigator of the GOAL trial. “These cases start in childhood, but the sore throats and fevers get missed. The healthcare system is looking for malaria, tuberculosis and HIV.”
Now, the public health system has evidence that a widely available and highly affordable treatment can change the life course for affected children: penicillin.
Prevention Trial Shows Promising Results
The GOAL trial was conducted in Northern Uganda from July 2018 through October 2020 and involved 818 children ages 5-17 years with latent rheumatic heart disease. The participants either received penicillin injections every four weeks for two years, or no treatment. All participants underwent echocardiography screening at the start and end of the trial.
Detailed results were published Nov. 13, 2021, in the New England Journal of Medicine. Beaton and co-authors reported that just three participants (0.8%) who received penicillin experienced latent rheumatic heart disease progression after two years, compared to 33 (8.3%) who didn’t receive the treatment. Prior to this study, it was unknown if antibiotics were effective at preventing the progression of latent rheumatic heart disease.
The prevention results are important because people across Uganda with latent rheumatic heart disease who develop irreversible valve damage have little or no access to valve surgery, Okello says.
Importantly, unlike many other pathogens that have developed resistance to older antibiotics, penicillin remains effective against Group A strep bacteria.
Global Collaboration Makes Impact
Beaton and Okello collaborated with scientists from more than a dozen institutions based in nations including the U.S., Uganda, Australia, India, Mozambique, France, South Africa, and Brazil to conduct the study.
“This was the first contemporary randomized controlled trial in rheumatic heart disease,” Beaton says. “The results are incredibly important on their own, but also demonstrate that high-quality clinical trials are feasible to address this neglected cardiovascular disease.”
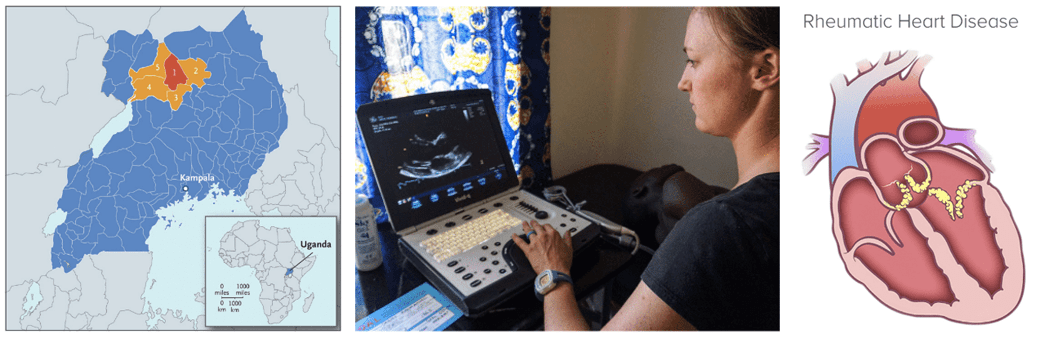
Left: Map showing GOAL study locations in Uganda. Middle: While children were treated near their homes, analyzing study data involved international collaboration. Right: How rheumatic fever can damage the heart.
Next Challenge: Building a Screening System
While penicillin itself is low-cost, much more work is needed in Uganda and other low-resource nations to make echocardiogram screenings more accessible for children. Hurdles include setting up clinics, addressing transportation issues, and overcoming a limited public understanding of the disease.
However, establishing improved screening programs will likely be more affordable than the infrastructure required to provide heart valve re-placement surgery, Beaton notes. While partners in Uganda work to find infrastructure funding, Beaton will lead a five-year follow-up study called “GOAL Post.” It remains unclear how long monthly injections should continue, especially once a per-son’s heart appears to return to normal.
“That study will look at the durability of prophylaxis in preventing adverse outcomes as well as determining whether it is safe for children to stop antibiotic prophylaxis once their heart returns to normal,” Beaton says.
The team has received NIH funding for a related project called “ADUNU”—which means “heart” in Luo—that will support developing and evaluating district-wide programs, including active case finding with echocardiography and registry-based care using a mobile platform developed at Cincinnati Children’s. The team also has applied for funding for a study to evaluate the use of oral vs. injected penicillin, which may be more practical in low-resource settings.
While the research focused on Uganda, the findings have implications across sub-Saharan Africa and beyond. “Anywhere there’s poverty, or fractured healthcare systems, or poor access to primary healthcare, you can find rheumatic heart disease,” Beaton says.
Ugandan children participating in the GOAL rheumatic fever study.
About the Study
The inspiration for this research dates back more than a decade to when Beaton and Okello were cardiology fellows at Children’s National Hospital in Washington, DC. “I was really lucky to get plugged into the Uganda Heart Institute team. Once I got to go over there, I saw first-hand the enormous need, so we worked together to develop this research program,” Beaton says.
Funding sources for this study included the Thrasher Research Fund, Gift of Life International, Children’s National Hospital Foundation, the Elias–Ginsburg Family, Wiley Rein, Philips Foundation, AT&T Foundation, Heart Healers International, the Karp Family Foundation, Huron Philanthropies, and the Cincinnati Children’s Heart Institute Research Core.
Also contributing to the study were researchers from the University of Cincinnati College of Medicine; Makerere University, Uganda; Children’s National Hospital, Washington, DC; The Royal Children’s Hospital, Melbourne; Telethon Kids Institute, Western Australia; Virginia Tech Carilion School of Medicine; Université de Paris; Instituto Nacional de Saude, Mozambique; Universidade Federal de Minas Gerais, Brazil; Emory University School of Medicine, Atlanta; Starship Children’s Hospital, Auckland; Geisel School of Medicine, New Hampshire; Red Cross Children’s Hospital, South Africa; and the All-India Institute of Medical Sciences.
Citation
Beaton A, Okello E, Rwebembera J, Grobler A, Engelman D, Alepere J, Canales L, Carapetis J, DeWyer A, Lwabi P, Mirabel M, Mocumbi AO, Murali M, Nakitto M, Ndagire E, Nunes MCP, Omara IO, Sarnacki R, Scheel A, Wilson N, Zimmerman M, Zühlke L, Karthikeyan G, Sable CA, Steer AC. Secondary Antibiotic Prophylaxis for Latent Rheumatic Heart Disease. N Engl J Med. 2022 Jan 20;386(3):230-240.




