
Gurjit "Neeru" Khurana Hershey, MD, PhD
- Director, Division of Asthma Research
- Co-Director, Office of Pediatric Clinical Fellowships
- Professor, UC Department of Pediatrics
- gurjit.hershey@cchmc.org
- Board Certified
About
Biography
I was drawn to discovery and science early in my academic career. At the University of Iowa, under the guidance of my mentor Peter Rubinstein, PhD, I submitted an abstract on my undergraduate research and was selected to present a poster at the Federation of American Societies for Experimental Biology (FASEB) meeting in California.
There, at my first scientific meeting, I listened to keynote speakers and Nobel Prize winners Michael S. Brown, MD, and Joseph L. Goldstein, MD. I was mesmerized by the impact of their work and energized at the possibility of a career in clinically relevant medical research. I approached the podium after their presentation, seeking career-path advice. At their suggestion, I immediately began researching universities with dual-degree programs and was accepted to the National Institutes of Health (NIH)-funded Medical Scientist Training Program (MSTP) at Washington University School of Medicine.
As a young scientist, research, for me, was less about the specific question I was trying to answer and more about the excitement and passion for discovery. Over time — and after seeing the impact of asthma on my own family — my research interests became focused on allergic disorders.
Here at Cincinnati Children’s Hospital Medical Center, my lab combines epidemiologic, basic, translational and clinical research approaches to answer fundamental questions related to childhood asthma, atopic dermatitis, food allergy and allergic rhinitis. I’m joined by a diverse group of talented individuals with distinct backgrounds and skillsets, all working around our shared mission to improve the lives of children with allergic disorders.
Over the past two decades, we have published over 180 articles and established several large longitudinal population cohorts focused on asthma and allergic disorders, including the first U.S. cohort of children with atopic dermatitis. For the last 14 years, I’ve served as the principal investigator of an NIH-funded Asthma and Allergic Diseases Cooperative Research Center (AADCRC) — one of only 11 in the country — and I currently serve as the chair of the AADCRC steering committee.
Current work in my lab is focused on:
- Understanding the role of the epithelial barrier in the pathogenesis of atopic dermatitis, food allergy, asthma and allergic diseases
- Delineation of the mechanistic basis of the atopic march
- Molecular phenotyping and endotyping of allergic diseases to better define and subclassify atopic dermatitis and asthma disease phenotypes to improve prediction and management of these common disorders
- Identifying and testing new treatments for allergic diseases, especially asthma
I was honored in 2019 to be recognized for my work with a Daniel Drake Medal from the University of Cincinnati (UC) College of Medicine, the college’s highest honor. That same year, my alma mater, Washington University Medical School, presented me with their Alumni Achievement Award. In 2018, Cincinnati Children’s recognized me with their Senior Faculty Award for Research Achievement, and in 2015, I was awarded the World Allergy Organization Scientific Achievement Award.
I’m humbled by this recognition, but perhaps the most rewarding aspect of my career has been training young scientists and my involvement with our MSTP here at Cincinnati Children’s and the UC College of Medicine.
Research is the engine that drives innovation. We need people to understand both sides of the equation — research and clinical medicine — to advance medicine and discover new therapeutics and technologies. Graduates of MD/PhD programs are leaders who can impact change and improve health.
I was extremely proud in 2012 to be named director of our MSTP and look forward to continuing to nurture and develop these leaders.
I have also been fortunate to extend my leadership to a number of roles within my scientific community. I previously directed the Ohio Children’s Hospitals Research Collaborative Asthma Initiative, which encompasses the six major children’s hospitals across the state. In addition, I was a member of the National Advisory Allergy and Infectious Disease Council, served on the Board of Directors for the American Board of Allergy and Immunology, and held a role on the Editorial Board of the Journal of Allergy and Clinical Immunology.
For over 20 years, my team and I have worked tirelessly to improve the health of children. After all, the roots of most diseases, including allergic disorders, are in childhood. This only amplifies the potential of our work. Although we have made great strides, there is a lot of work to be done in terms of our understanding of allergic disorders. By focusing on the health of children, I believe we are guaranteeing a healthier, better future.
BS: University of Iowa, Iowa City, IA, 1985,
PhD: Washington University School of Medicine, St. Louis, MO, 1990,
MD: Washington University School of Medicine, St. Louis, MO, 1992,
Residency: St. Louis Children's Hospital, St. Louis, MO, 1995,
Fellowship: St. Louis Children's Hospital, St. Louis, MO, 1997,
Services and Specialties
Research Areas
Additional Languages
PunjabiLocation
Insurance Information
Cincinnati Children's strives to accept a wide variety of health plans. Please contact your health insurance carrier to verify coverage for your specific benefit plan.
Publications
Disease-associated KIF3A variants alter gene methylation and expression impacting skin barrier and atopic dermatitis risk. Nature Communications. 2020; 11(1):4092.
Identification of two early life eczema and non-eczema phenotypes with high risk for asthma development. Clinical and Experimental Allergy. 2019; 49(6):829-837.
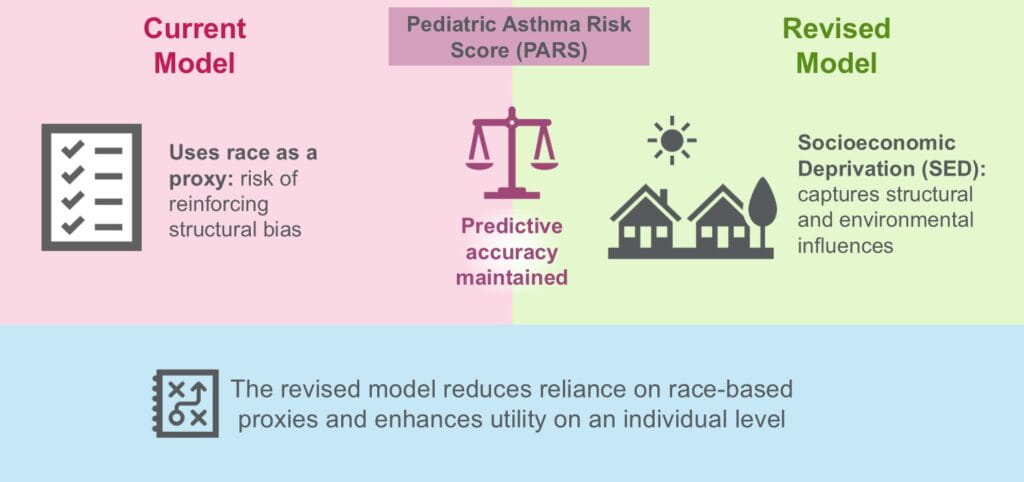
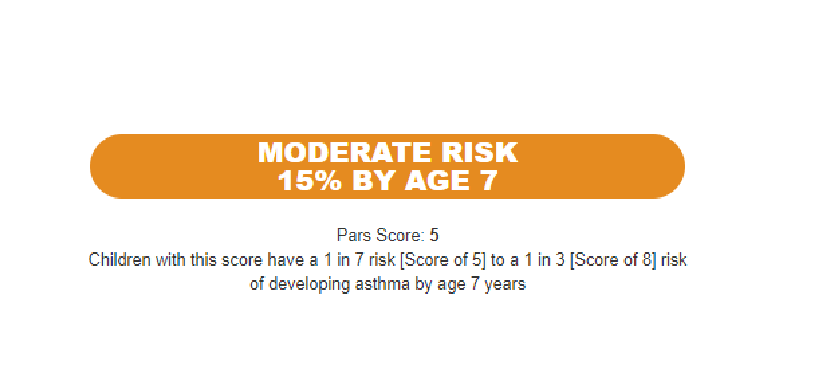
A Pediatric Asthma Risk Score to better predict asthma development in young children. Journal of Allergy and Clinical Immunology. 2019; 143(5):1803-1810.e2.
Environmental exposures and mechanisms in allergy and asthma development. Journal of Clinical Investigation. 2019; 129(4):1504-1515.
Vitamin D supplementation attenuates asthma development following traffic-related particulate matter exposure. Journal of Allergy and Clinical Immunology. 2019; 143(1):386-394.e3.
GENEASE: real time bioinformatics tool for multi-omics and disease ontology exploration, analysis and visualization. Bioinformatics. 2018; 34(18):3160-3168.
Ohio Pediatric Asthma Repository: Opportunities to Revise Care Practices to Decrease Time to Physiologic Readiness for Discharge. Hospital pediatrics. 2018; 8(6):305-313.
High number of early respiratory infections in association with allergic sensitization to mold promotes childhood asthma. Journal of Allergy and Clinical Immunology. 2018; 141(5):1921-1924.e4.
Contribution of an impaired epithelial barrier to the atopic march. Annals of Allergy, Asthma and Immunology. 2018; 120(2):118-119.
Staphylococcal Biofilms in Atopic Dermatitis. Current Allergy and Asthma Reports. 2017; 17(12):81.
From the Blog
A ‘Must Read’—An Update on Asthma Prediction
Gurjit Khurana Hershey, MD, PhD, Jocelyn M. Biagini, PhD ...1/21/2026
Childhood Wheeze Patterns Linked to Distinct Asthma Subtypes Later in Life
Gurjit Khurana Hershey, MD, PhD7/9/2025
Omitting Race from Lung Function Equations Increases Detection of Asthma in Black Children
Gurjit Khurana Hershey, MD, PhD, Jocelyn M. Biagini, PhD2/28/2025
Study Pierces a Mystery of Healthy Skin Barrier Formation
Gurjit Khurana Hershey, MD, PhD8/7/2024
Overactive Natural Killer Cells Linked to Asthma Progression
Gurjit Khurana Hershey, MD, PhD, Stephen N. Waggoner, PhD2/9/2024
Asthma Risk Score Tool Performs Well Across Diverse Populations
Gurjit Khurana Hershey, MD, PhD, Jocelyn M. Biagini, PhD8/11/2023







Patient Ratings and Comments
All patient satisfaction ratings and comments are submitted by actual patients and verified by a leading independent experience management company, Qualtrics. Patient identities are withheld to ensure confidentiality and privacy. Only those providers whose satisfaction surveys are administered through Cincinnati Children’s Hospital Medical Center are displayed. Click here to learn more about our survey