Rapid Research Establishes Key Diagnostic Tool for COVID-Related MIS-C
Published June 2021 | Lancet Rheumatology
Early in the COVID-19 pandemic, the impact on children was relatively small compared to older adults. But for the children who did suffer severe illness, one of the most serious concerns was multisystem inflammatory syndrome (MIS-C).
Initially, this condition appeared similar to the inflammatory disorders Kawasaki disease and macrophage activation syndrome (MAS), both of which were familiar to experts at Cincinnati Children’s. So what was different about MIS-C and could this form of hyperinflammation be diagnosed and controlled with similar approaches?
A team led by first author Jackeline Rodriguez-Smith, MD, MSc, RhMSUS, and Grant Schulert, MD, PhD, was quickly assembled to find out.
Between April 30, 2019, and Dec. 14, 2020, the team enrolled 19 patients with MIS-C and nine with Kawasaki disease. While both groups displayed similar levels of several inflammatory biomarkers including S100 proteins and Interleukin-18, those with MIS-C had significantly higher median concentrations of IFNγ-induced CXCL9—1730 pg/mL vs. 278 pg/mL. The MIS-C patients with elevated CXCL9 also tended to have signs of shock, acute kidney injury, altered mental status, myocardial dysfunction and other biomarkers of severe illness.
This set of symptoms more closely resembled MAS, which is also an IFNγ-driven disorder, and suggests more-specific approaches for diagnosis and management.
“These findings have two key implications,” Schulert says. “First, diagnosing MIS-C will become harder with more people having prior COVID infection and the disease becoming more endemic. CXCL9, especially if the turnaround time is short, may be very helpful. Second, this tells us that treatment approaches used in macrophage activation syndrome - such as blocking key inflammatory cytokines - may be very helpful in the most severe MIS-C cases.”
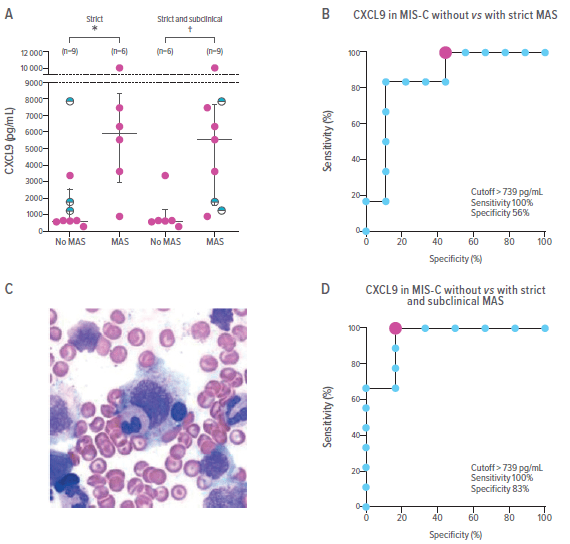
Differential CXCL9 Concentrations in MIS-C with and without MAS
Panel (A) shows CXCL9 concentrations in patients with MIS-C based only on strict MAS classification criteria (left) and including subclinical MAS (right). The subclinical MAS data appears as half-filled black circles. Panel (B) shows ROC curves for CXCL9 differentiation based on strict criteria. The red dot indicates the optimal cutoff point. Panel (C) A bone marrow biopsy smear of a patient with MIS-C shows haemophagocytosis with an ingested lymphocyte and a myeloid precursor in the process of being ingested by a histocyte. Panel (D) a ROC curve for CXCL9 differentiation that includes subclinical MAS. The red dot indicates the optimal cutoff point. ROC=receiver operating characteristic. MAS=macrophage activation syndrome. MIS-C=multisystem inflammatory syndrome in children.